What Is The Gold Standard Treatment For Enlarged Prostate

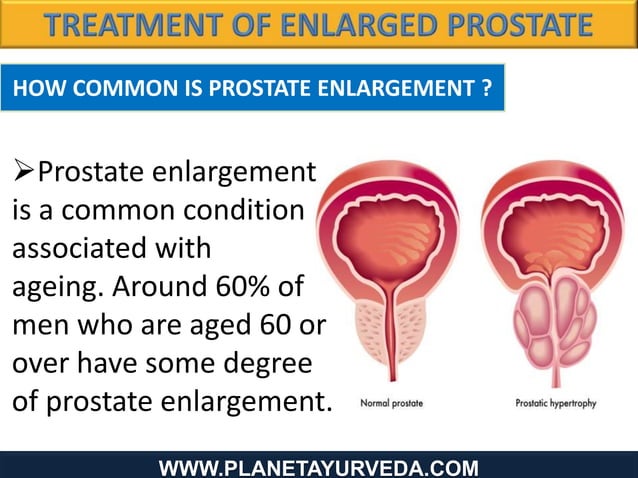
Imagine waking up multiple times during the night, not to the gentle sounds of nature, but to the insistent urge to urinate. For many men, this isn't an occasional inconvenience; it's a nightly reality caused by an enlarged prostate, a condition known as Benign Prostatic Hyperplasia (BPH). This seemingly small gland can have a significant impact on quality of life, turning restful nights into restless ones.
The "gold standard" treatment for BPH is a subject of ongoing discussion and evolution. While there's no single cure-all, Transurethral Resection of the Prostate (TURP) has historically held that title due to its proven efficacy and long-term results. However, less invasive options are increasingly challenging its dominance, offering men a wider range of choices to address their specific needs and preferences.
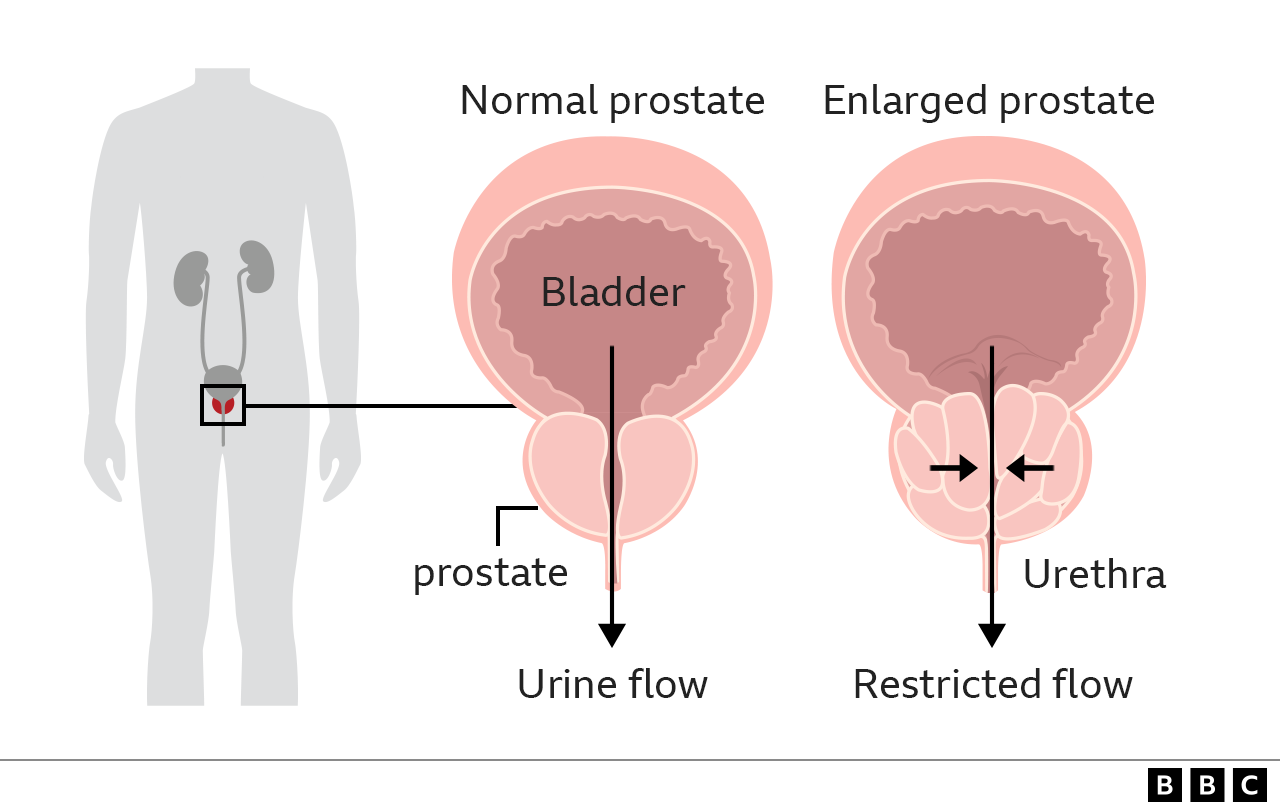
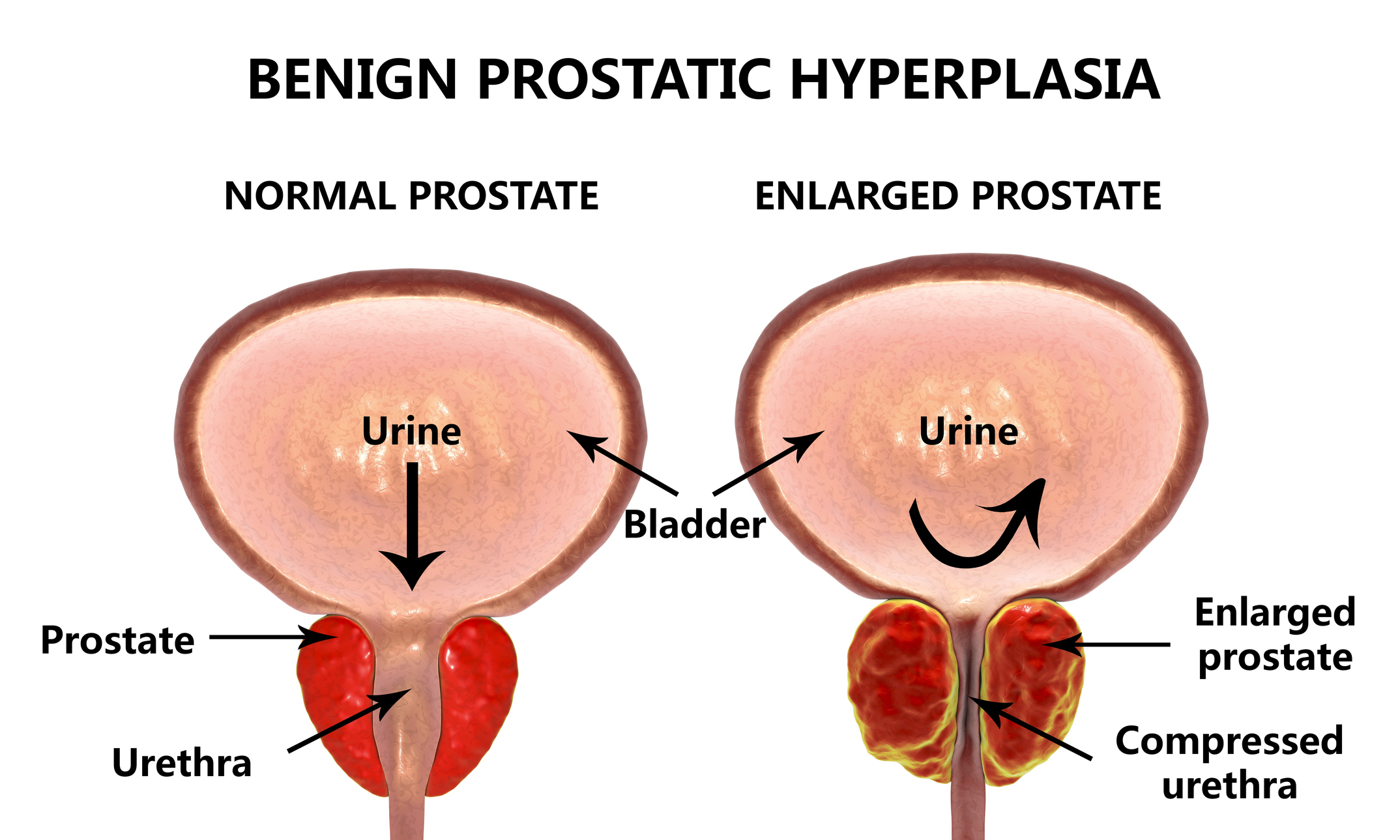
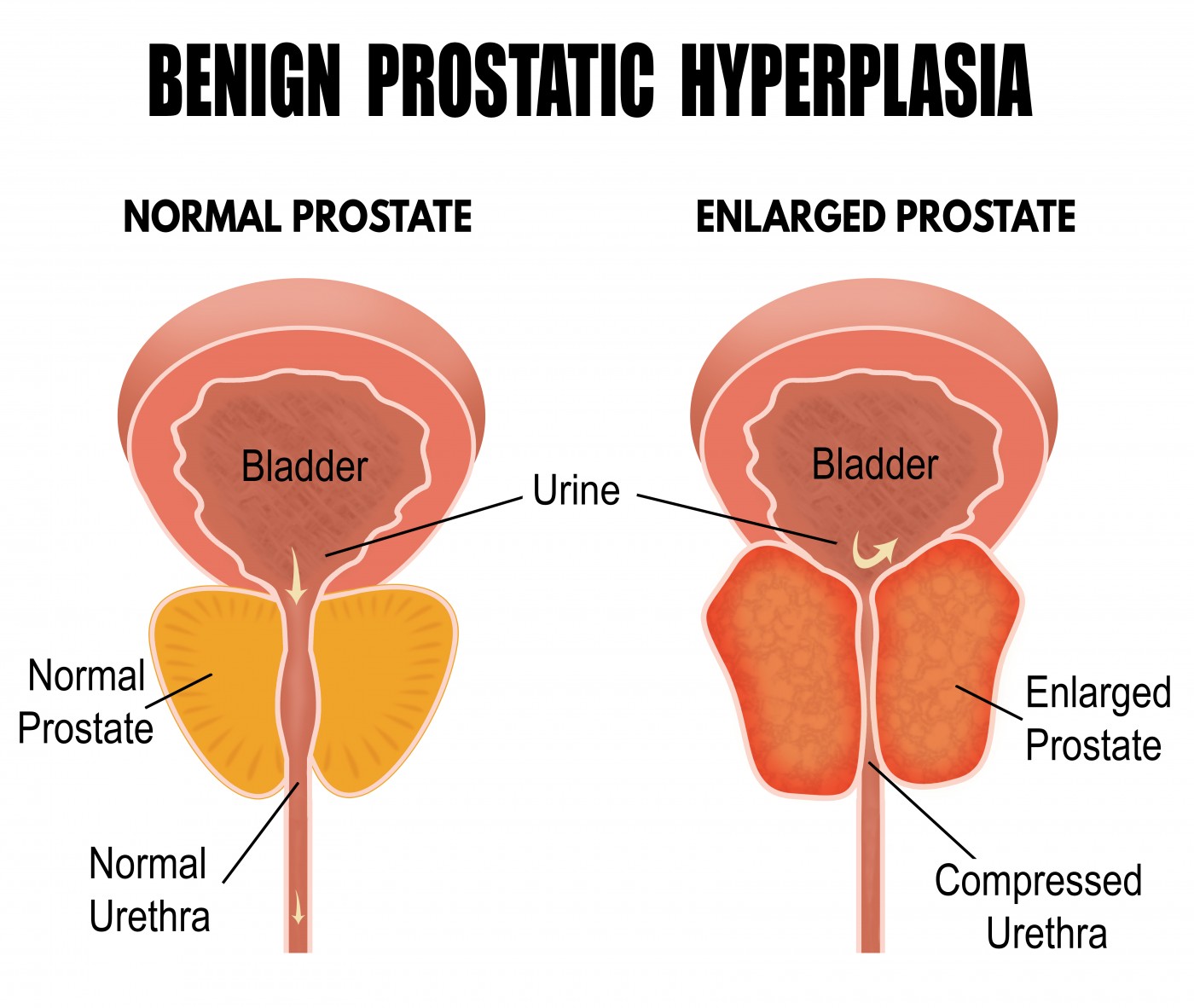
Understanding Benign Prostatic Hyperplasia
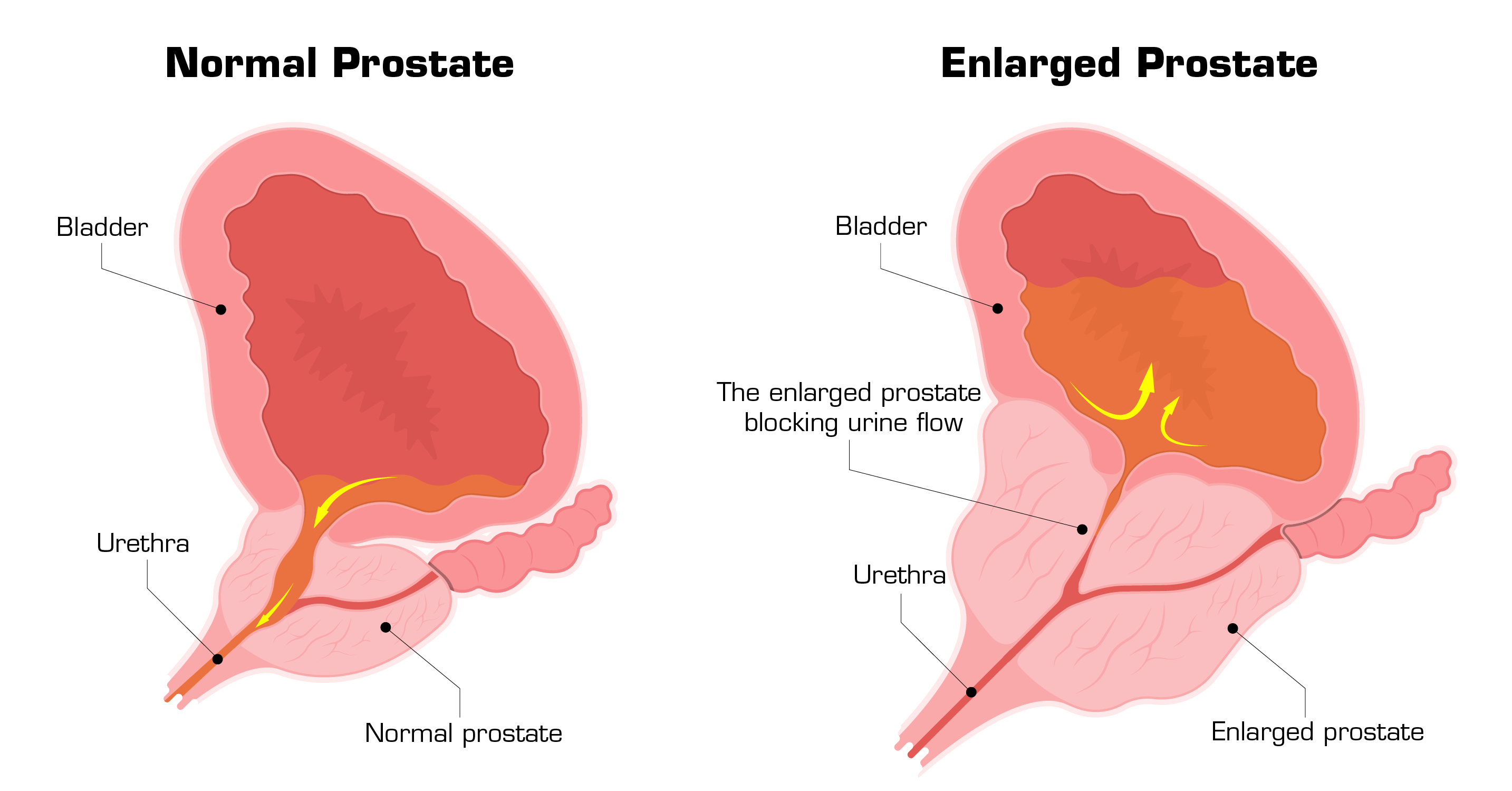
BPH, though common as men age, isn’t cancerous. It’s characterized by the non-cancerous enlargement of the prostate gland, which surrounds the urethra, the tube that carries urine from the bladder. As the prostate grows, it can squeeze the urethra, making it difficult to urinate and leading to a variety of bothersome symptoms.
These symptoms include frequent urination, especially at night (nocturia), urgency, a weak urine stream, difficulty starting urination, and incomplete emptying of the bladder. The severity of these symptoms varies greatly from person to person. For some, it’s a mild inconvenience, while for others, it significantly impacts their daily lives.
The Historical Gold Standard: TURP
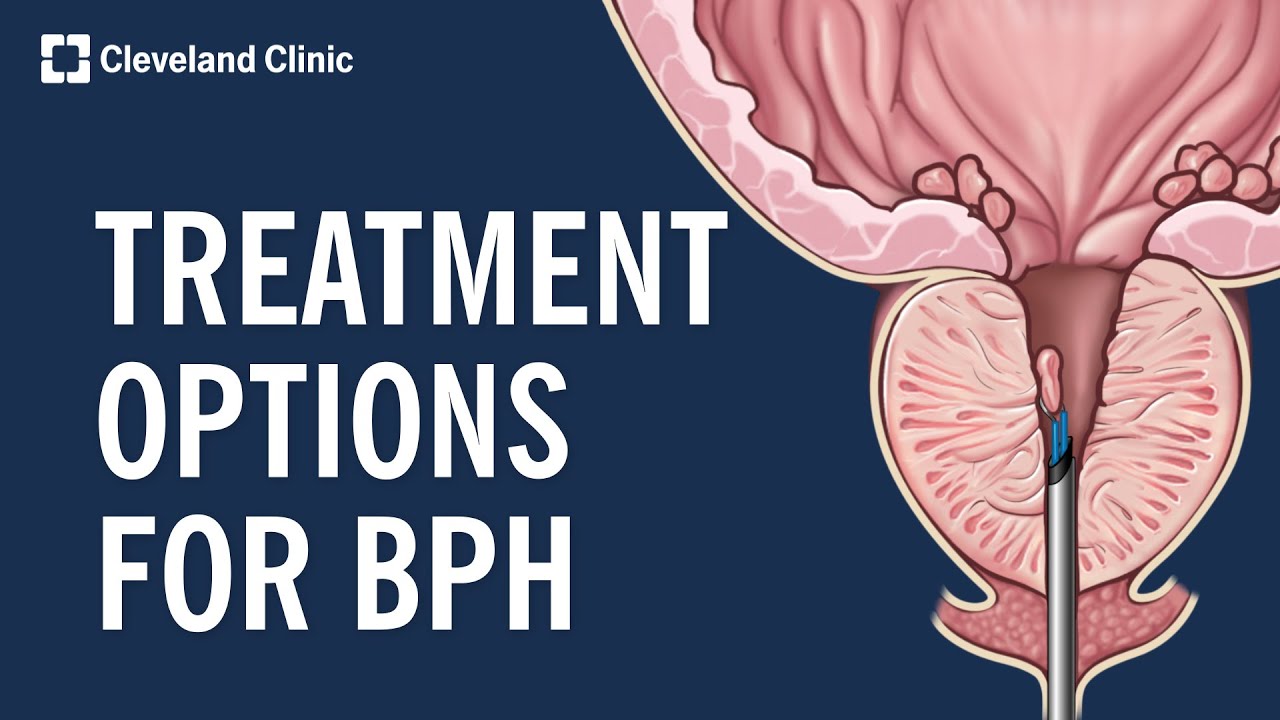
TURP involves surgically removing the obstructing prostate tissue through the urethra. No external incision is required, making it less invasive than open surgery. This procedure has been around for decades and boasts a high success rate in relieving BPH symptoms.
During a TURP procedure, a resectoscope is inserted through the urethra to the prostate. The surgeon then uses an electrical loop to carefully cut away excess prostate tissue. The removed tissue is flushed out, and the urethra is left open for easier urine flow.
While highly effective, TURP isn't without potential side effects. These can include bleeding, infection, urinary incontinence, erectile dysfunction, and retrograde ejaculation (where semen flows backward into the bladder during ejaculation). These risks, though relatively low, have fueled the search for less invasive alternatives.
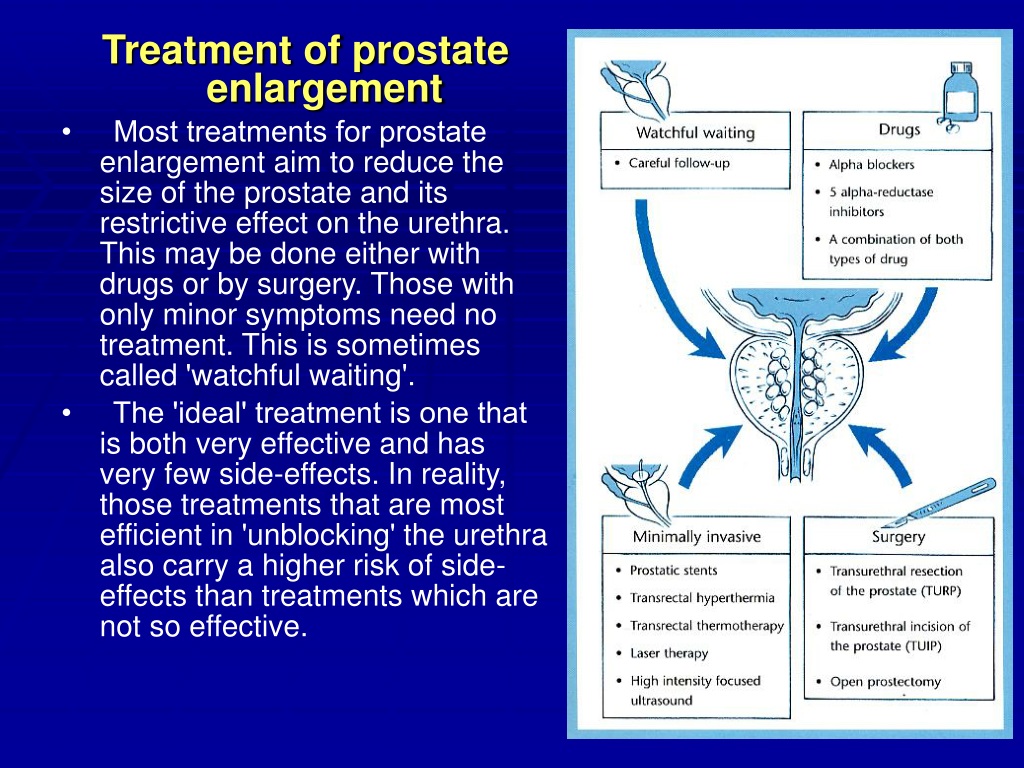
Challenging the Throne: Minimally Invasive Procedures
In recent years, several minimally invasive surgical techniques (MISTs) have emerged as alternatives to TURP. These procedures aim to relieve BPH symptoms with less tissue damage, faster recovery times, and fewer side effects.
Transurethral Microwave Thermotherapy (TUMT) uses microwave energy to heat and destroy excess prostate tissue. Another option, Transurethral Needle Ablation (TUNA), employs radiofrequency energy to achieve a similar effect.
Prostatic Urethral Lift (PUL), such as the UroLift system, involves placing small implants to compress the enlarged prostate tissue and open up the urethra. This procedure is particularly attractive because it preserves sexual function in most men.
Water Vapor Therapy (Rezūm) uses sterile water vapor (steam) to ablate prostate tissue. The steam is injected into the prostate, causing the cells to die and shrink the gland.
Laser Therapy, including Holmium Laser Enucleation of the Prostate (HoLEP) and Photoselective Vaporization of the Prostate (PVP), uses lasers to either remove or vaporize excess prostate tissue. These laser techniques often result in less bleeding compared to TURP.
These MISTs offer distinct advantages, but it’s crucial to understand their limitations. While they generally have fewer side effects and shorter recovery times, their long-term effectiveness may not be as well-established as TURP. The best option depends on the individual's specific situation, including the size of the prostate, the severity of symptoms, and overall health.
Medical Management: Medications as a First Line of Defense
Before considering surgery, many men explore medical management options. Medications can help manage BPH symptoms effectively.
Alpha-blockers, such as tamsulosin (Flomax) and alfuzosin (Uroxatral), relax the muscles in the prostate and bladder neck, making it easier to urinate. 5-alpha reductase inhibitors, such as finasteride (Proscar) and dutasteride (Avodart), shrink the prostate gland over time by blocking the hormone dihydrotestosterone (DHT).
Combination therapy, using both alpha-blockers and 5-alpha reductase inhibitors, is also common. Cialis (tadalafil), a medication primarily used for erectile dysfunction, is also approved to treat BPH symptoms. These medications don't cure BPH, but they can provide significant relief from symptoms.
Lifestyle Modifications and Complementary Therapies
In addition to medical and surgical interventions, certain lifestyle modifications can help manage BPH symptoms. These include limiting fluid intake before bedtime, avoiding caffeine and alcohol, and practicing "double voiding" (waiting a few minutes after urinating and then trying again).
Some men explore complementary therapies, such as saw palmetto, pygeum, and rye grass pollen extract. However, the scientific evidence supporting their effectiveness is mixed, and it's essential to discuss these options with a healthcare provider before use.
The Evolving Definition of the "Gold Standard"
The concept of a "gold standard" is dynamic and evolving. While TURP has a long track record of success, the rise of MISTs and effective medications has broadened the landscape of BPH treatment. The ideal approach is now highly individualized.
The American Urological Association (AUA) provides guidelines for the management of BPH. These guidelines emphasize a shared decision-making process between the patient and their doctor. Together, they can weigh the benefits, risks, and long-term outcomes of each treatment option to determine the best course of action.
Factors such as the patient's age, overall health, prostate size, symptom severity, and personal preferences all play a role in the decision. Furthermore, the availability of specific technologies and the surgeon's expertise can influence treatment choices.
A Future of Personalized Care
The future of BPH treatment is moving towards personalized care. Advances in diagnostic imaging and molecular profiling may one day allow doctors to tailor treatment plans based on an individual's specific characteristics and disease progression. This could involve selecting the most appropriate surgical technique or predicting which patients are most likely to benefit from a particular medication.
Ultimately, managing BPH is about improving quality of life. By staying informed about the available treatment options and working closely with a healthcare provider, men can find the best solution to alleviate their symptoms and reclaim their nights.
The journey to finding relief from BPH symptoms can feel daunting. However, with a better understanding of the various treatment options and the support of experienced medical professionals, men can navigate this condition and live fulfilling lives, free from the constant disruption of frequent urination.