Which Endovascular Procedure Reopens Narrowed Blood Vessels
.jpg)
For individuals suffering from the debilitating effects of narrowed blood vessels, a minimally invasive procedure known as angioplasty offers a beacon of hope. This endovascular technique has revolutionized the treatment of various vascular conditions, providing a less invasive alternative to traditional surgery.
Angioplasty, often performed in conjunction with stenting, is a procedure used to widen narrowed or blocked blood vessels, most commonly arteries. It is a crucial intervention for patients experiencing conditions like atherosclerosis, where plaque buildup restricts blood flow. This article delves into the details of angioplasty, its significance, and its impact on patients' lives.
Understanding Angioplasty: The Mechanics of Reopening Vessels
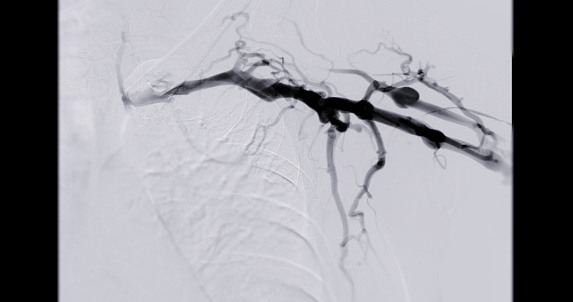
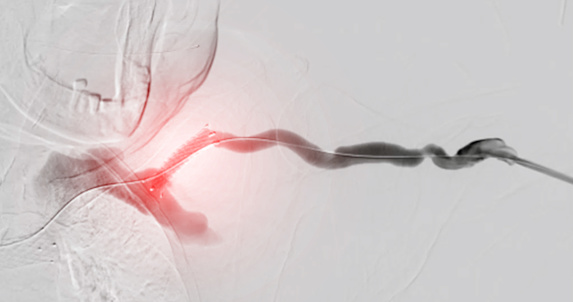
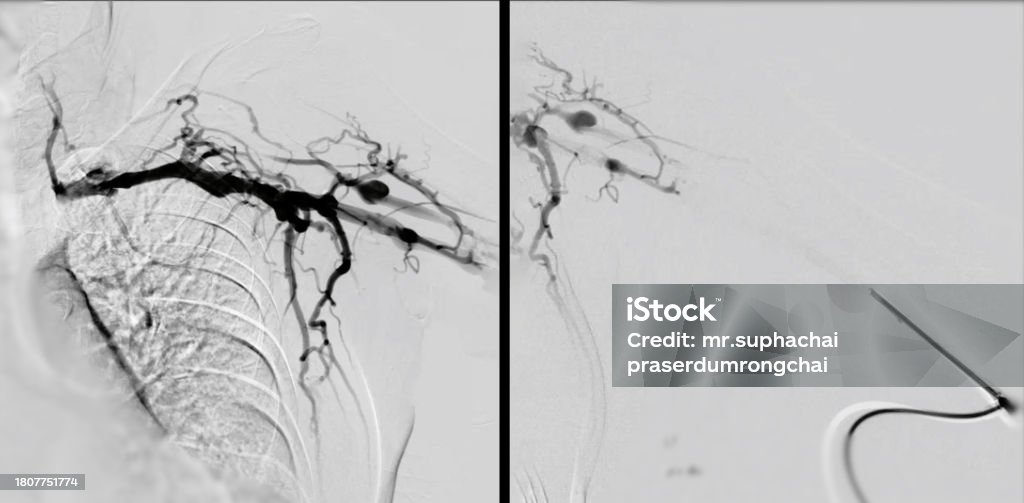
Angioplasty involves inserting a thin, flexible tube called a catheter into a blood vessel, typically in the arm or groin. Guided by imaging techniques such as X-ray fluoroscopy, the catheter is advanced to the site of the blockage or narrowing.
Once in position, a balloon at the tip of the catheter is inflated. This inflation compresses the plaque against the artery wall, widening the vessel and improving blood flow.
In many cases, a stent, a small mesh tube, is then deployed to provide scaffolding and keep the artery open after the balloon is deflated and removed. Stents can be made of bare metal or coated with medication to prevent re-narrowing of the artery, a process known as restenosis.
The Significance of Angioplasty in Modern Medicine
The significance of angioplasty lies in its ability to restore blood flow to vital organs and tissues. It reduces the risk of serious complications like heart attack, stroke, and limb ischemia. According to the American Heart Association, angioplasty is a life-saving procedure for many patients with coronary artery disease.
Furthermore, angioplasty is a minimally invasive procedure, meaning it involves smaller incisions and less trauma to the body compared to open surgery. This translates to shorter hospital stays, faster recovery times, and reduced pain for patients.
“Angioplasty has dramatically changed the landscape of vascular care,” says Dr. Emily Carter, a leading interventional cardiologist at Massachusetts General Hospital. “It allows us to treat blockages effectively and efficiently, improving patients’ quality of life and preventing serious cardiovascular events.”
Who Benefits from Angioplasty?
Angioplasty is typically recommended for individuals with significant narrowing or blockage of arteries causing symptoms such as chest pain (angina), shortness of breath, leg pain (claudication), or dizziness. It is also used in emergency situations, such as during a heart attack, to quickly restore blood flow to the heart muscle.
Patients diagnosed with peripheral artery disease (PAD), carotid artery disease, or renal artery stenosis may also be candidates for angioplasty. Each condition presents unique challenges and requires careful evaluation to determine the suitability of the procedure.
The decision to proceed with angioplasty is made after a thorough evaluation by a healthcare team, including cardiologists, vascular surgeons, and interventional radiologists. Factors such as the severity of the blockage, the patient's overall health, and the presence of other medical conditions are taken into consideration.
A Patient's Perspective: Regaining Quality of Life
For many patients, angioplasty is more than just a medical procedure; it is a chance to regain their quality of life. John Smith, a 62-year-old retired teacher, experienced debilitating leg pain due to PAD.
“I could barely walk a block without stopping,” John recounts. "After angioplasty and stenting, I can now walk without pain, play with my grandchildren, and enjoy life again."
His experience highlights the transformative impact of angioplasty on individuals struggling with vascular disease.
Potential Risks and Complications
While angioplasty is generally a safe procedure, it is not without risks. Potential complications include bleeding or infection at the catheter insertion site, damage to the blood vessel, allergic reaction to contrast dye, and restenosis (re-narrowing of the artery).
The risk of complications is relatively low, especially when the procedure is performed by experienced interventionalists in well-equipped medical centers. Patients are closely monitored during and after the procedure to detect and manage any potential issues.
The use of drug-eluting stents has significantly reduced the risk of restenosis compared to bare-metal stents. Careful patient selection and adherence to post-procedure medication regimens are also crucial in minimizing complications.
Looking Ahead: Advancements in Endovascular Technology
The field of endovascular technology is constantly evolving, with ongoing research and development focused on improving angioplasty techniques and outcomes. Newer stent designs, drug-coated balloons, and advanced imaging technologies are being developed to enhance the precision and effectiveness of the procedure.
Furthermore, researchers are exploring novel approaches to prevent restenosis and reduce the need for repeat procedures. These advancements hold promise for further improving the long-term outcomes for patients undergoing angioplasty.
Angioplasty stands as a testament to the power of medical innovation in improving the lives of countless individuals. As technology continues to advance, the future of endovascular interventions holds even greater potential for treating vascular disease and enhancing patient well-being.