Which Of The Following Accelerated The Use Of Value-based Care
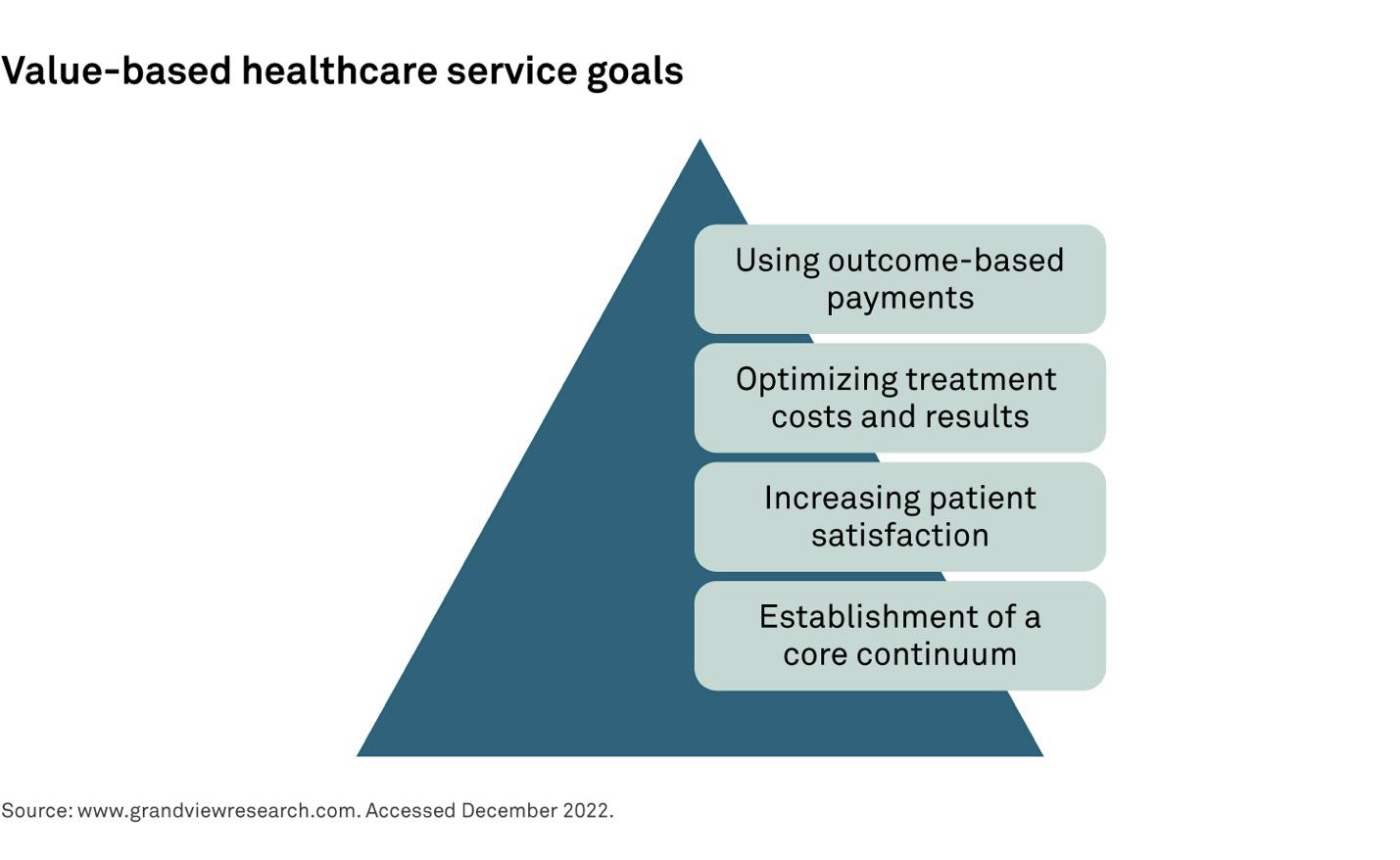
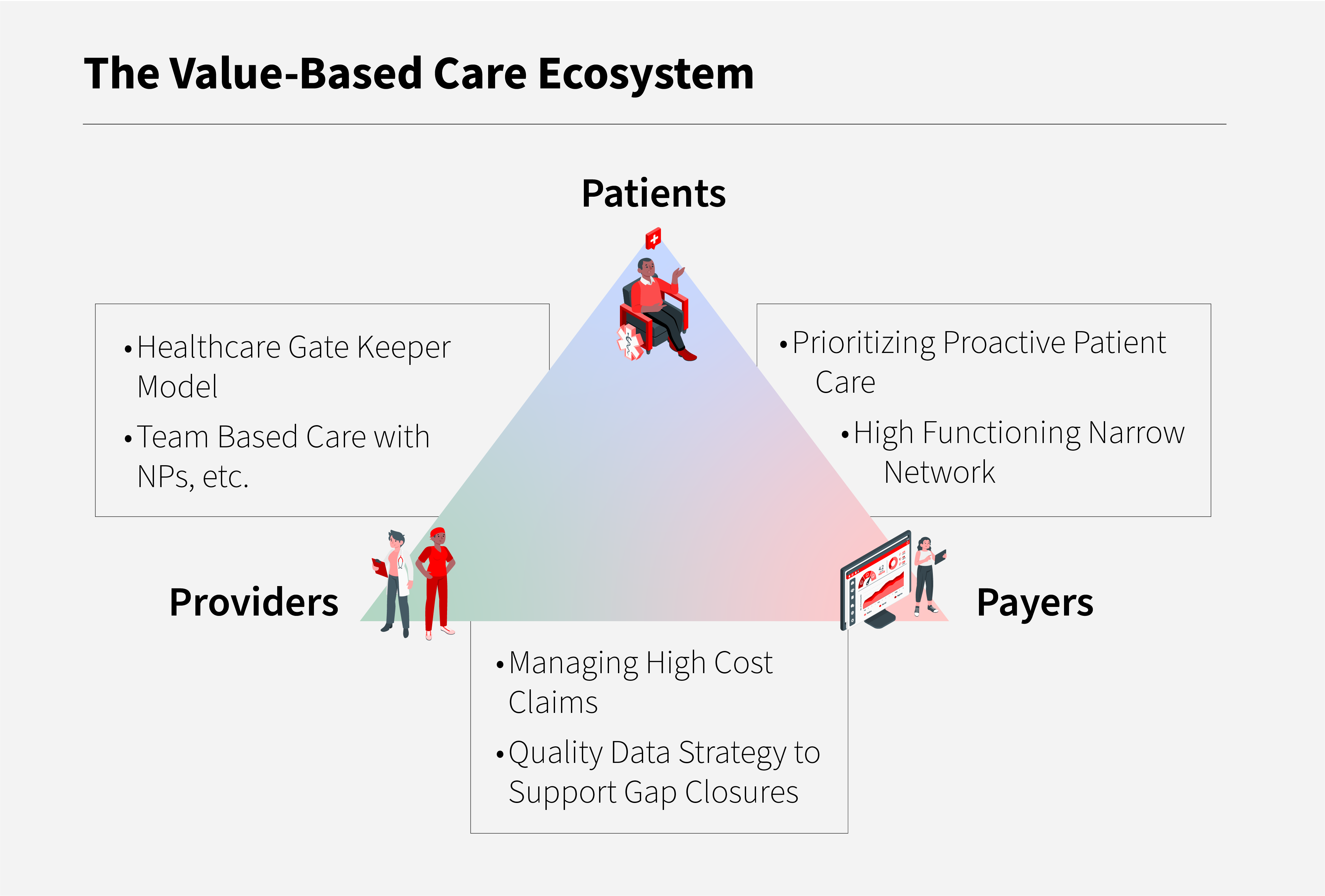
The shift towards value-based care (VBC) is accelerating, driven by a confluence of factors reshaping healthcare delivery and reimbursement models. A perfect storm of policy changes, technological advancements, and market demands is pushing providers and payers towards prioritizing patient outcomes over volume.
This article examines the key catalysts behind the rapid adoption of VBC, focusing on specific initiatives and trends that have proven most impactful. We delve into the "who, what, where, when, why, and how" of this transformation, providing a clear and concise overview of the forces at play.
The Role of the Affordable Care Act (ACA)
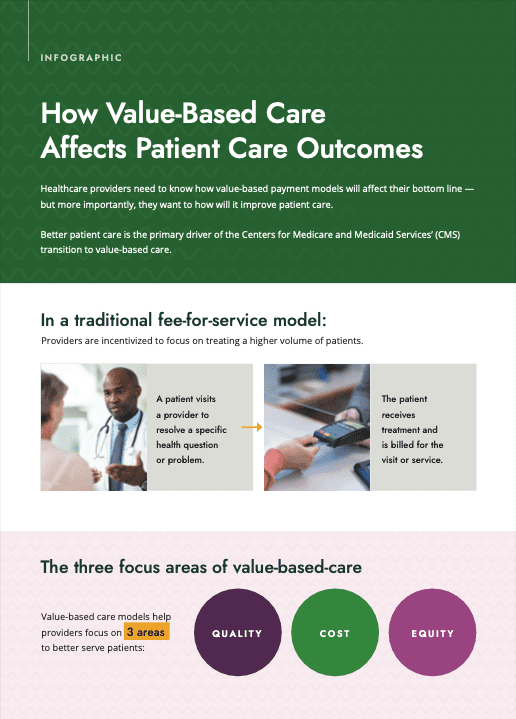
The Affordable Care Act (ACA), enacted in 2010, served as a major impetus for VBC adoption.
By emphasizing quality and cost-effectiveness, the ACA laid the groundwork for alternative payment models (APMs) that reward value over volume.
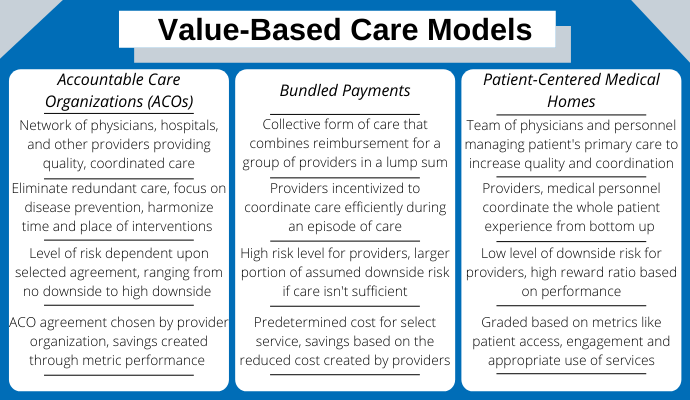
Specifically, the creation of Accountable Care Organizations (ACOs) within Medicare, as a direct result of the ACA, has incentivized providers to coordinate care and reduce unnecessary costs, significantly driving the shift toward VBC.
MACRA and the Move to APMs
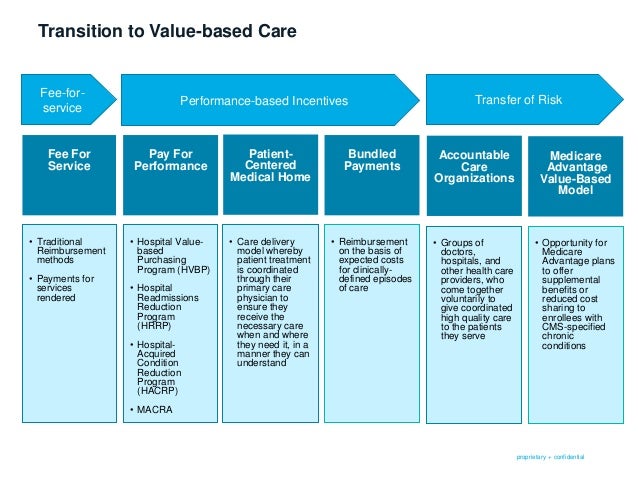
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) further amplified the focus on VBC.
MACRA repealed the Sustainable Growth Rate (SGR) formula and established the Quality Payment Program (QPP), which includes two tracks: Advanced APMs and the Merit-based Incentive Payment System (MIPS).
Through financial incentives and penalties, MACRA encourages providers to participate in APMs, accelerating the transition to VBC by tying reimbursement to quality and performance metrics.
Technological Advancements as Enablers
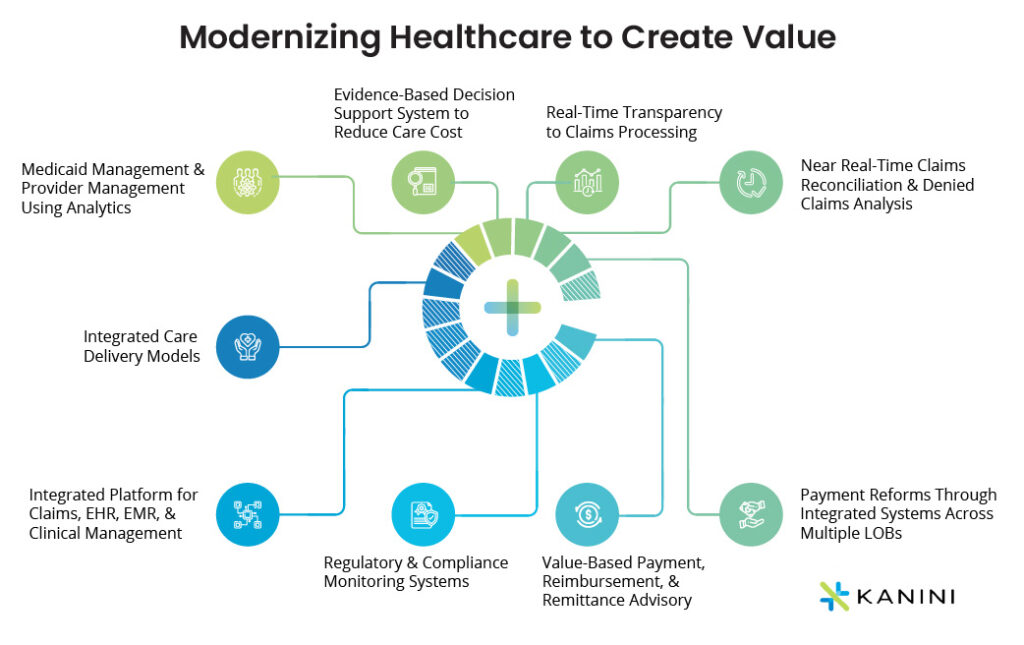
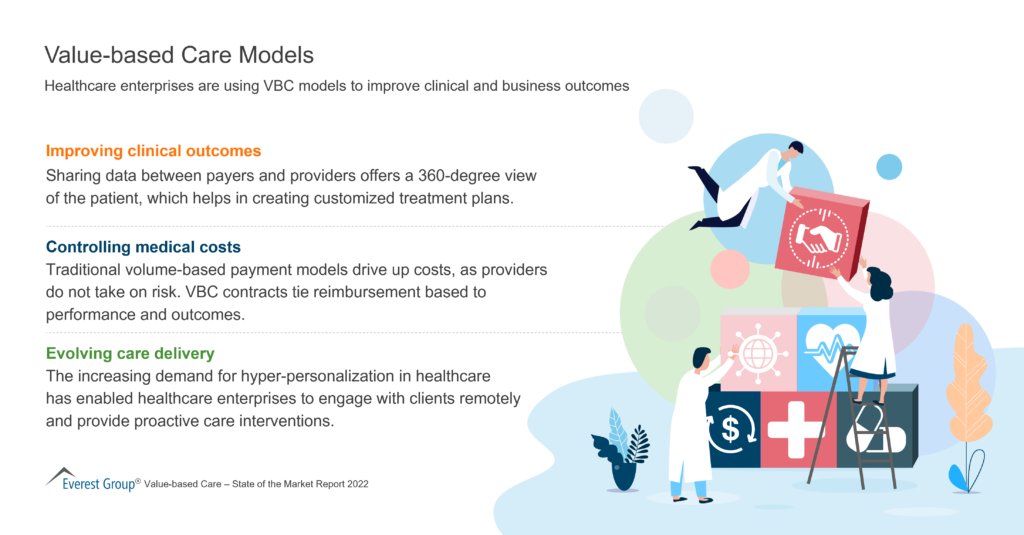
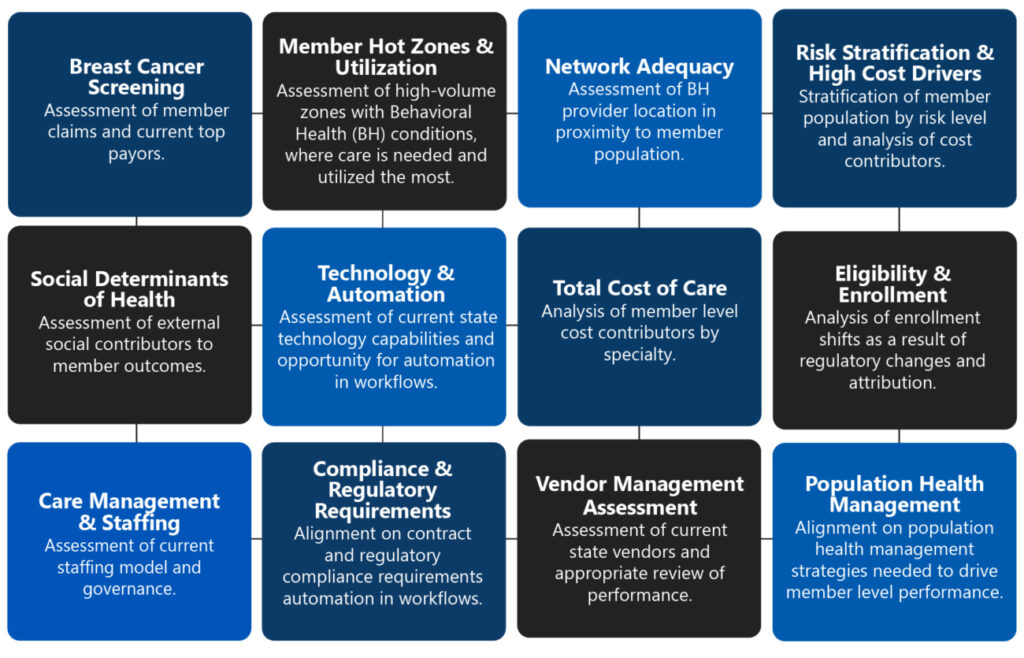
Advancements in health information technology (HIT) have played a crucial role in facilitating VBC.
Electronic Health Records (EHRs), data analytics platforms, and telehealth solutions provide the tools necessary to collect, analyze, and share patient data effectively.
This enhanced data transparency and interoperability enable providers to better manage patient populations, identify high-risk individuals, and deliver personalized care, essential components of a VBC model.
The Rise of Consumerism in Healthcare
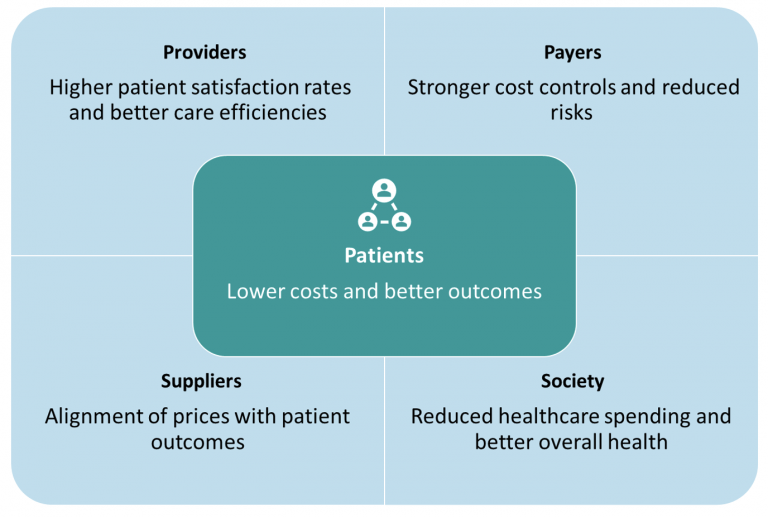
Increasingly, patients are becoming more active consumers of healthcare.
They are demanding greater transparency in pricing and quality, and are seeking out providers who prioritize patient experience and outcomes.
This shift in consumer expectations is driving providers to adopt VBC principles in order to attract and retain patients in a competitive market.
Employer-Sponsored Health Plans
Employers, who bear a significant portion of healthcare costs, are also pushing for VBC.
Seeking ways to control expenses and improve employee health, many employers are contracting directly with providers or offering incentives for employees to choose high-value care options.
This employer-driven demand for VBC is creating further momentum for its adoption across the healthcare landscape. The Business Group on Health, which represents large employers, has actively promoted VBC strategies.
The Impact of COVID-19
The COVID-19 pandemic exposed vulnerabilities in the traditional fee-for-service system and highlighted the importance of coordinated, proactive care.
The pandemic also accelerated the adoption of telehealth and remote patient monitoring, further enabling VBC delivery models.
Moreover, the increased focus on public health and preventive care during the pandemic has reinforced the value proposition of VBC in promoting population health and reducing healthcare disparities.
Specific Examples of VBC Implementation
Numerous healthcare systems and organizations are successfully implementing VBC models.
Kaiser Permanente, for instance, has long been a leader in integrated care delivery, demonstrating the benefits of coordinating care and aligning incentives to improve patient outcomes and reduce costs.
Other examples include Geisinger Health System's ProvenCare program and the numerous ACOs participating in Medicare's Shared Savings Program.
Challenges and Obstacles
Despite the growing momentum, challenges remain in fully implementing VBC.
Data interoperability issues, resistance to change from some providers, and the complexity of measuring and attributing value can hinder progress.
Addressing these challenges requires ongoing investment in technology, education, and collaboration among all stakeholders.
Looking Ahead: The Future of VBC
The shift towards VBC is expected to continue in the coming years.
As healthcare costs continue to rise and the demand for quality and value increases, payers and providers will have even greater incentives to embrace VBC models.
Ongoing efforts to refine payment models, improve data analytics, and engage patients will be crucial in realizing the full potential of VBC to transform healthcare delivery and improve patient outcomes. Government regulations and incentives will continue to shape the landscape.