Which Of The Following Is An Antineoplastic Agent

The fight against cancer is a constant, evolving battle, relying heavily on the development and application of antineoplastic agents. Choosing the right agent for a specific cancer type and patient profile is crucial. Misunderstanding or misidentification can lead to ineffective treatment and potentially harmful side effects, underscoring the need for clarity and accurate information.
This article aims to clarify what constitutes an antineoplastic agent, offering a definitive guide based on scientific consensus and established medical practice. It will delve into the classification, mechanisms of action, and considerations surrounding these vital medications. The goal is to provide a comprehensive understanding, aiding healthcare professionals, patients, and anyone seeking reliable information on cancer treatment.
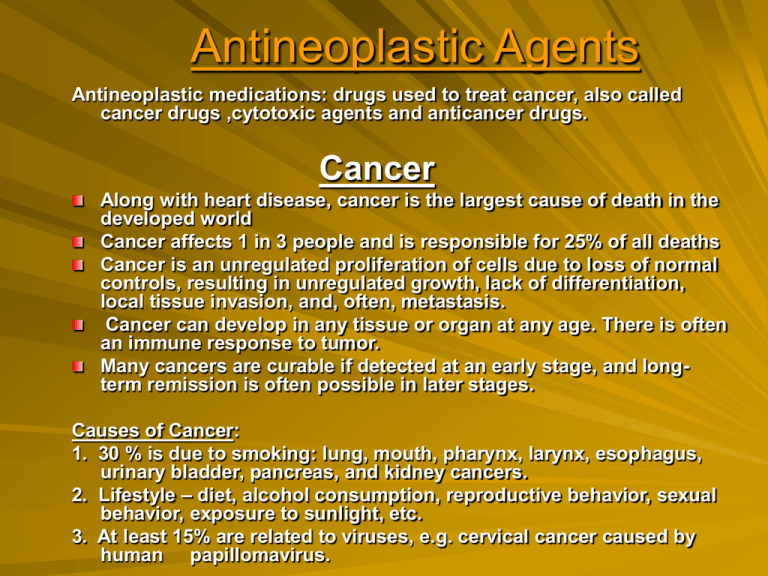
What Defines an Antineoplastic Agent?
An antineoplastic agent, at its core, is any substance that inhibits or prevents the growth and spread of neoplasms, commonly known as tumors or cancers. These agents are the cornerstone of chemotherapy, radiation therapy, and targeted cancer therapies. Their efficacy lies in their ability to disrupt the processes that allow cancer cells to proliferate uncontrollably.
The term encompasses a broad range of compounds, acting through diverse mechanisms. They can include synthetic chemicals, naturally derived compounds, and even biological agents like antibodies. The specific action of an antineoplastic drug dictates its effectiveness against different types of cancer.
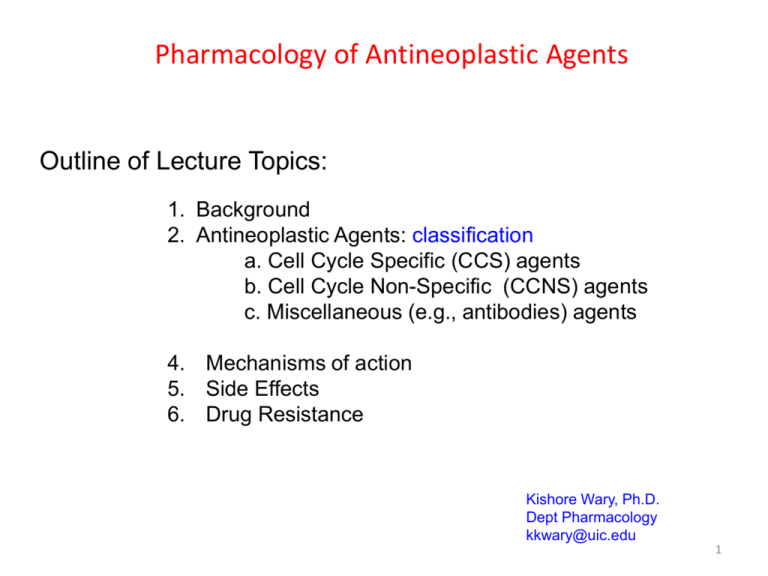
Classifying Antineoplastic Agents
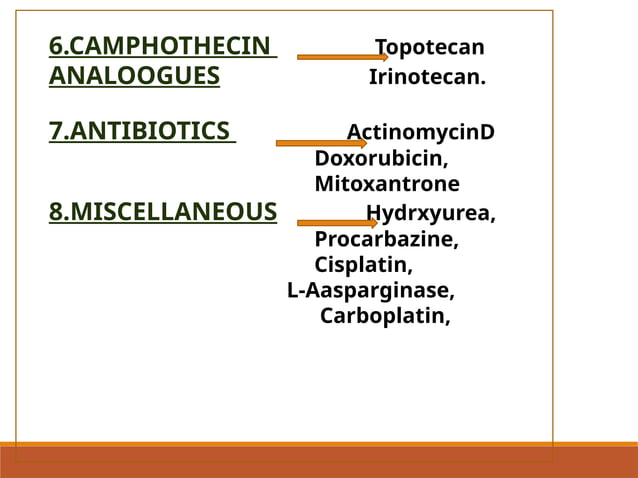
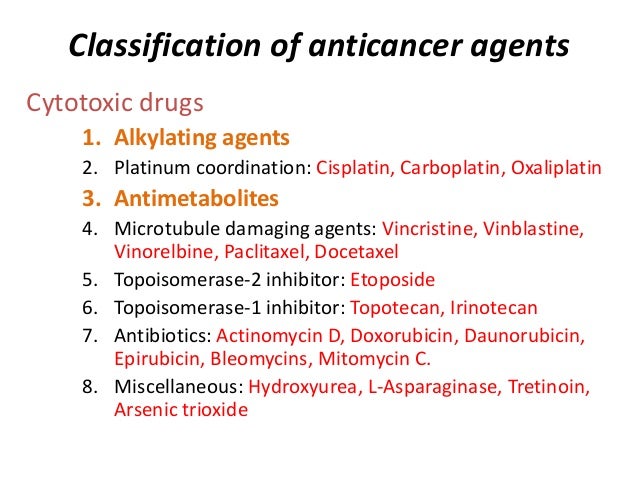
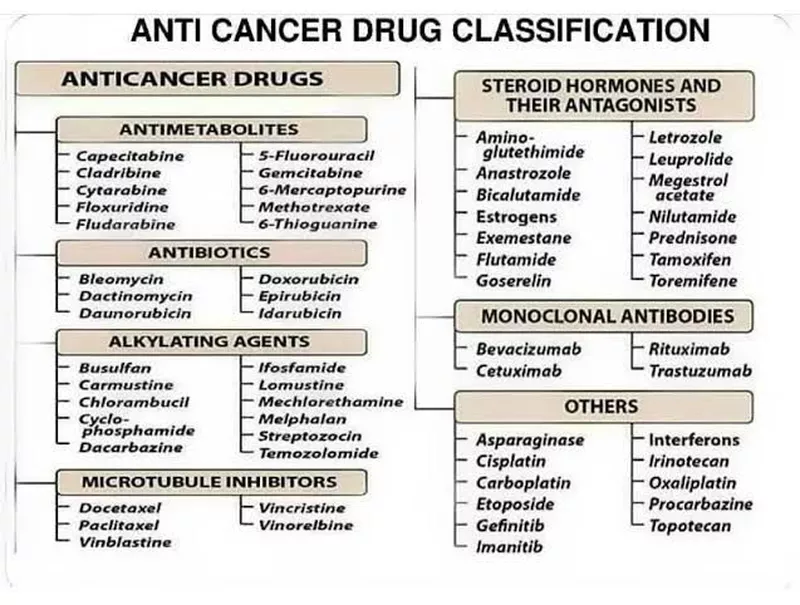
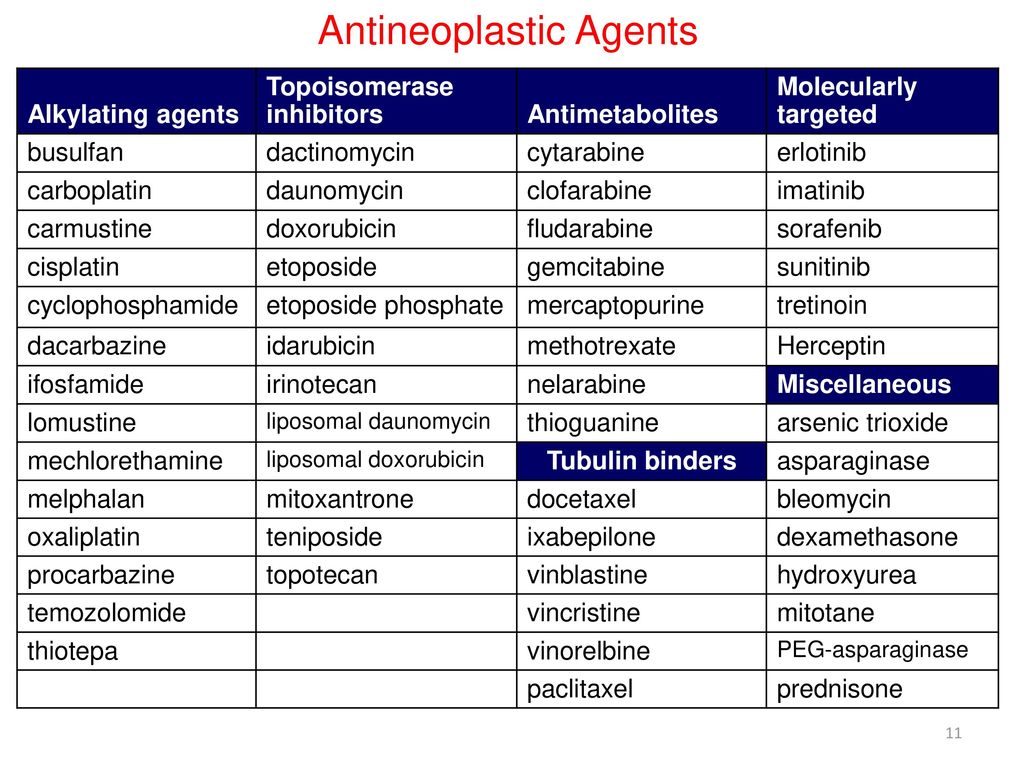
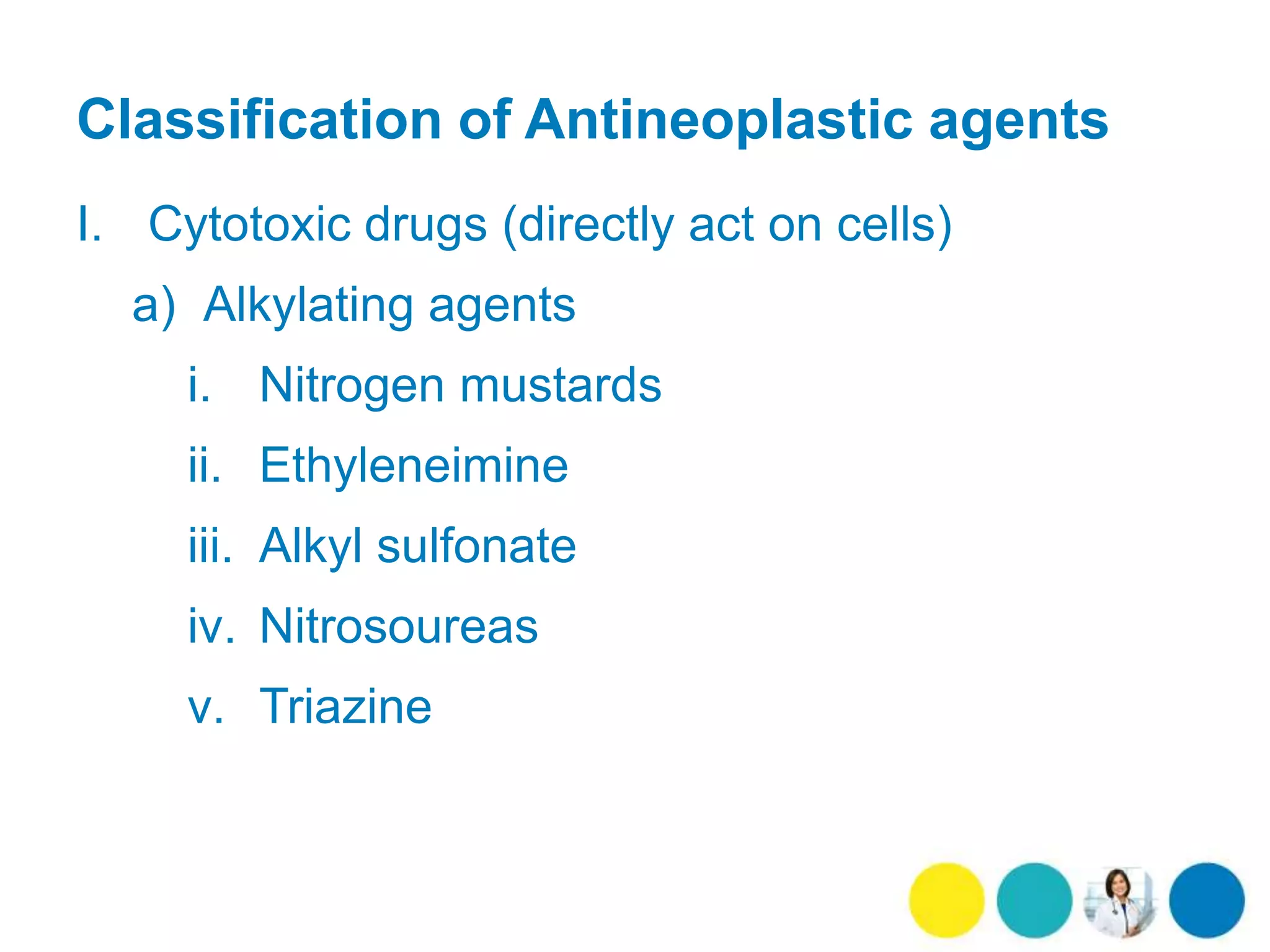
Antineoplastic agents are often categorized based on their mechanism of action. This classification helps oncologists choose the most appropriate treatment strategy. Key categories include alkylating agents, antimetabolites, antitumor antibiotics, topoisomerase inhibitors, mitotic inhibitors, and targeted therapies.
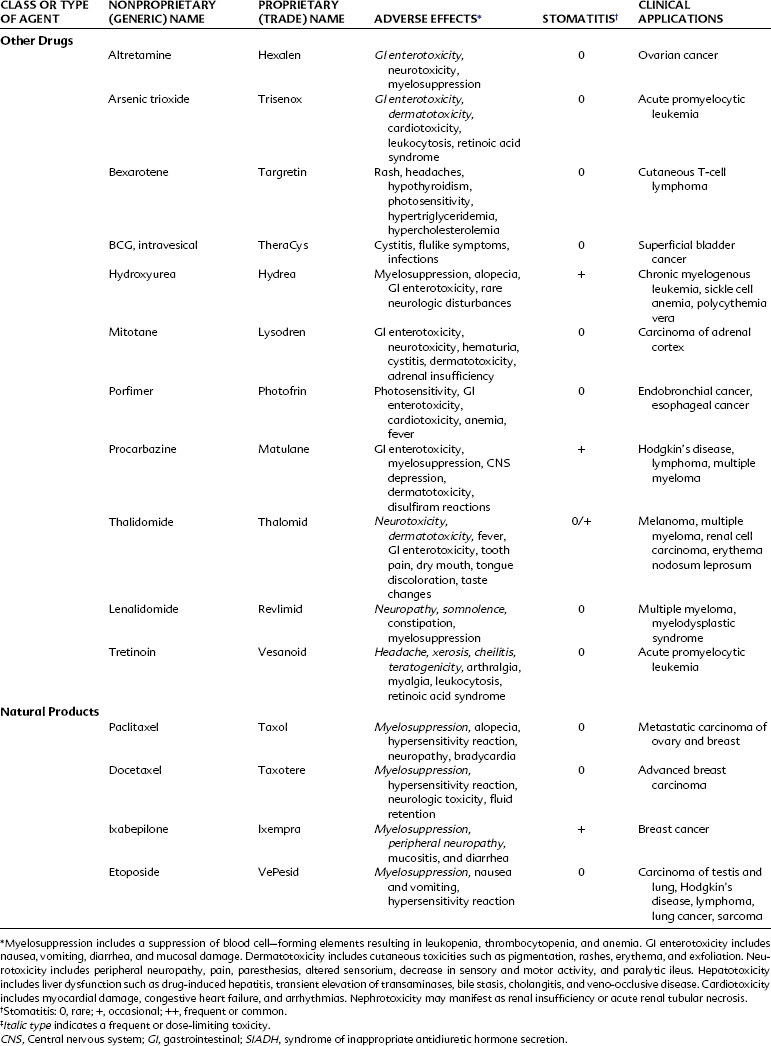
Alkylating agents directly damage DNA, preventing cell division. They are effective against a wide range of cancers, including leukemia, lymphoma, and certain solid tumors. However, they can also cause significant side effects due to their non-selective nature.
Antimetabolites interfere with the synthesis of DNA and RNA, essential components for cell growth. These agents mimic natural substances but disrupt metabolic processes. They are commonly used in treating leukemia, breast cancer, and colon cancer.
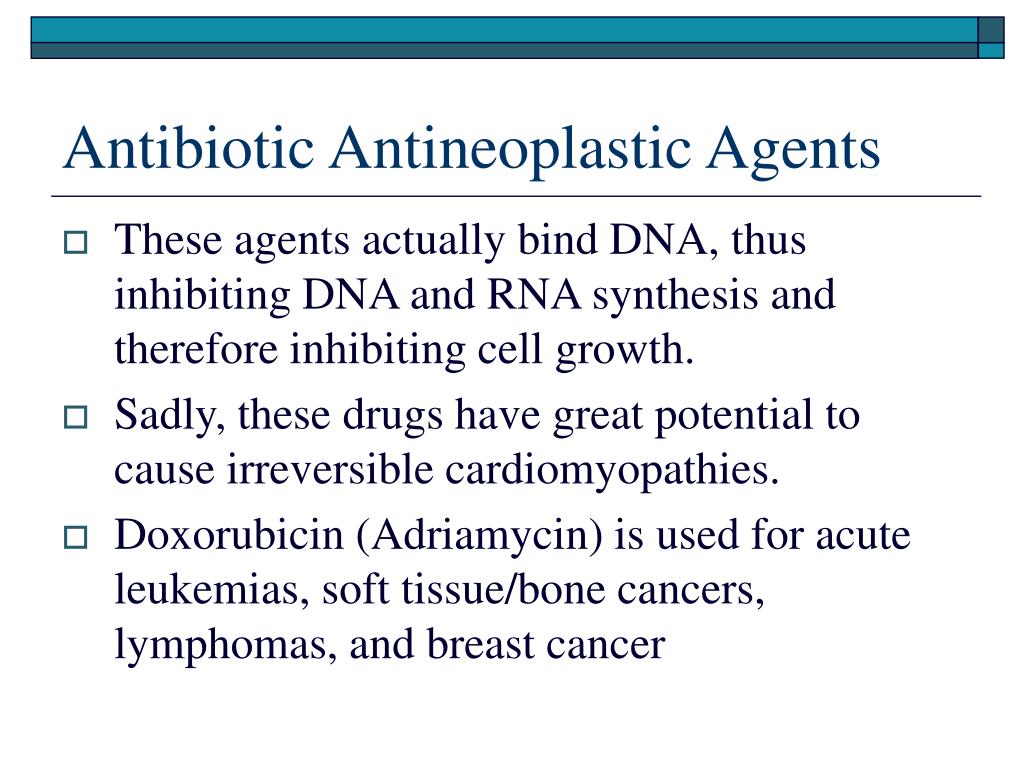
Antitumor antibiotics are derived from microbial sources and have cytotoxic effects. They bind to DNA, disrupting its structure and function. These drugs are often used in combination with other antineoplastic agents to treat various cancers.
Topoisomerase inhibitors target enzymes that control DNA replication and repair. By interfering with these enzymes, these agents disrupt cell division. They are often used in the treatment of lung cancer, ovarian cancer, and certain types of leukemia.
Mitotic inhibitors interfere with cell division by disrupting the formation of microtubules. These drugs prevent cancer cells from dividing and multiplying. Examples include taxanes and vinca alkaloids, used in treating breast cancer, lung cancer, and lymphoma.
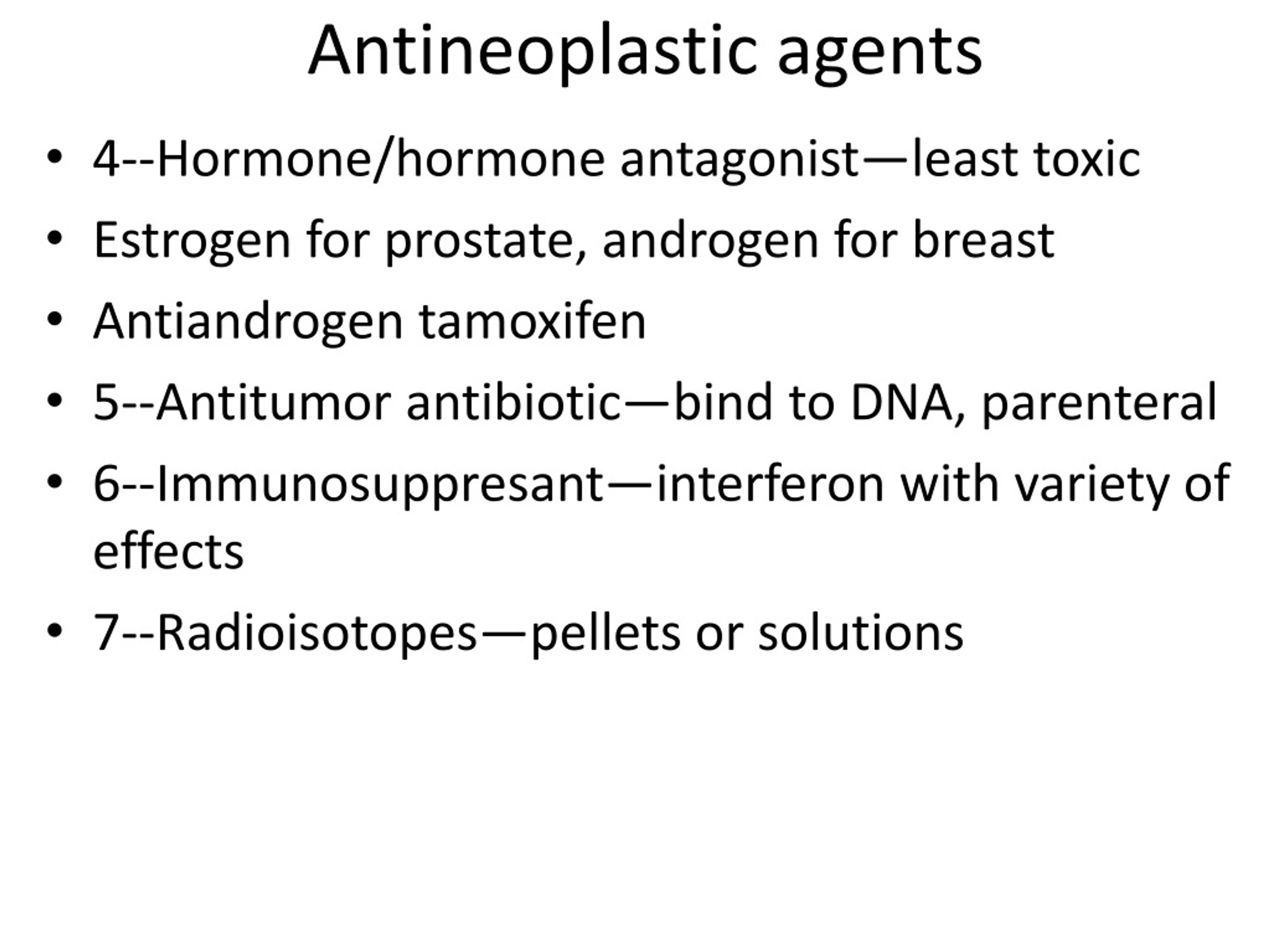
Targeted therapies represent a newer and more selective approach to cancer treatment. These agents target specific molecules or pathways involved in cancer cell growth and survival. Examples include monoclonal antibodies, tyrosine kinase inhibitors, and PARP inhibitors, offering a more personalized approach to cancer treatment.
Beyond Cytotoxicity: The Rise of Immunotherapy
While the term "antineoplastic agent" traditionally referred to cytotoxic drugs, the advent of immunotherapy has broadened its scope. Immunotherapy agents harness the body's immune system to fight cancer. These agents don't directly kill cancer cells but rather boost the immune response against them.
Immune checkpoint inhibitors, for instance, block proteins that prevent the immune system from attacking cancer cells. This approach has revolutionized the treatment of several cancers, including melanoma, lung cancer, and kidney cancer. Immunotherapy is often used in combination with other antineoplastic agents, such as chemotherapy, to achieve better outcomes.
Challenges and Considerations
The use of antineoplastic agents is not without its challenges. Many of these drugs have significant side effects, including nausea, fatigue, hair loss, and immunosuppression. The severity of side effects varies depending on the specific agent, dosage, and patient factors.
Furthermore, cancer cells can develop resistance to antineoplastic agents over time. This resistance can limit the effectiveness of treatment. Researchers are constantly working to develop new drugs and strategies to overcome drug resistance.
Personalized medicine is playing an increasingly important role in antineoplastic therapy. Genetic testing can help identify specific mutations in cancer cells, allowing oncologists to select the most effective targeted therapies. This approach aims to maximize treatment efficacy while minimizing side effects.
The Future of Antineoplastic Therapy
The field of antineoplastic therapy is rapidly evolving. New drugs and treatment approaches are constantly being developed and tested. Researchers are exploring novel targets and mechanisms of action to improve treatment outcomes and reduce side effects.
One promising area of research is the development of antibody-drug conjugates (ADCs). These agents combine the specificity of antibodies with the cytotoxic power of chemotherapy drugs. ADCs can selectively deliver chemotherapy drugs to cancer cells, minimizing damage to healthy tissues.
Another exciting development is the use of gene therapy to treat cancer. Gene therapy involves introducing new genes into cancer cells to make them more susceptible to treatment. This approach holds great promise for treating cancers that are resistant to conventional therapies. The journey of fighting cancer hinges upon the continuous evolution and advancement of antineoplastic agents.



.jpg)