Which Statement Is True Regarding Health Maintenance Organizations

In the complex landscape of healthcare, Health Maintenance Organizations (HMOs) occupy a significant, often debated, position. Understanding their operational principles and impact is crucial for both patients and policymakers. Recent discussions have centered on clarifying a specific statement regarding HMOs, seeking to address common misconceptions and promote informed decision-making.
This article will delve into the intricacies surrounding a central claim about HMOs. It will explore its validity based on available data and expert insights. The aim is to provide clarity on the features and functions of HMOs. It is also to empower individuals to navigate the healthcare system with greater understanding.
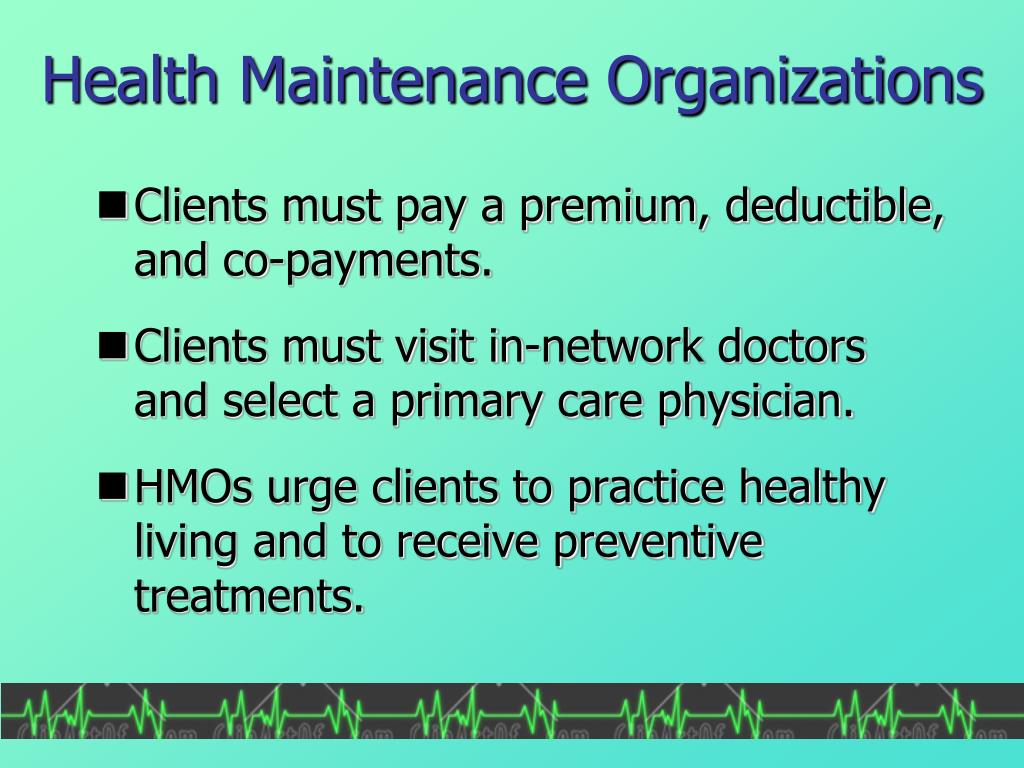
Defining the HMO Model
An HMO is a type of health insurance plan that typically limits coverage to care from doctors who work for or contract with the HMO. This network approach is a defining characteristic. It distinguishes HMOs from other insurance models like Preferred Provider Organizations (PPOs).
Unlike PPOs, HMOs usually require members to choose a primary care physician (PCP). The PCP acts as a gatekeeper, coordinating care and providing referrals to specialists within the HMO network. This gatekeeping function is designed to manage costs and ensure appropriate utilization of resources.
The Disputed Statement: Out-of-Network Coverage
The statement under scrutiny revolves around out-of-network coverage within an HMO. Specifically, the assertion that HMOs typically do not cover care received outside of their established network. Understanding the truth of this statement is vital for patients when selecting a health plan and seeking medical services.
According to the Centers for Medicare & Medicaid Services (CMS), HMOs generally restrict coverage to in-network providers. This restriction is a fundamental aspect of their cost-containment strategy. The idea is that negotiating discounted rates with a specific provider network allows HMOs to offer lower premiums to their members.
However, there are exceptions to this rule. Emergency care is typically covered regardless of whether the provider is in-network. In some cases, if a member needs a specialized service not available within the HMO network, the HMO may authorize out-of-network care.
Examining the Evidence
Data from various sources confirm that HMOs prioritize in-network care. A 2023 report by the Kaiser Family Foundation (KFF) found that the vast majority of HMO plans required members to seek care within the network to receive coverage. This trend aligns with the core principles of the HMO model.
Furthermore, studies have shown that HMOs often have lower out-of-pocket costs for members compared to PPOs, provided that care is received within the network. This cost advantage is a key selling point for many individuals when choosing an HMO plan.
It is important to note that some HMO plans may offer a "point-of-service" (POS) option. This allows members to seek care outside of the network, albeit at a higher cost. However, even with a POS option, in-network care is still incentivized and typically more affordable.
Exceptions and Special Circumstances
While HMOs primarily focus on in-network care, exceptions exist. Emergency services are a critical exception. Federal law mandates that emergency care must be covered regardless of network status, ensuring that individuals receive necessary treatment in urgent situations.
Another exception may arise when a member requires a specialized service that is not available within the HMO network. In such cases, the HMO may authorize out-of-network care after review and approval. This ensures that members receive necessary treatment even if it necessitates going outside the network.
These exceptions are designed to protect members and ensure access to essential healthcare services. However, it's crucial for members to understand the specific terms and conditions of their HMO plan to avoid unexpected costs.
Impact and Implications
The statement that HMOs generally do not cover out-of-network care is largely true, with specific exceptions. This understanding has significant implications for individuals choosing a health insurance plan. It also influences how they navigate the healthcare system.
For individuals who prioritize flexibility and the ability to see doctors outside of a network, an HMO might not be the best choice. PPOs, which offer greater out-of-network coverage (albeit at a higher cost), may be more suitable for these individuals.
However, for those who value lower premiums and are willing to adhere to the in-network requirements, an HMO can be a cost-effective option. It's crucial to weigh the pros and cons of each type of plan based on individual needs and preferences.
It is also important that consumers carefully review the details of their individual health plan. They should understand the specific rules regarding out-of-network coverage. This will allow them to make informed decisions about their healthcare and avoid unexpected expenses.
Conclusion
The claim that HMOs generally do not cover out-of-network care holds true, with exceptions for emergencies and certain specialized services. Recognizing this fundamental aspect of HMOs is crucial for both consumers and policymakers.
By understanding the limitations and benefits of HMOs, individuals can make informed decisions about their healthcare coverage. This will allow them to navigate the system effectively and achieve their health goals.
Further research and ongoing dialogue are essential to ensure that healthcare systems remain transparent, accessible, and responsive to the evolving needs of patients.

.jpg)
+-+Private.jpg)




.jpg)
.jpg)
+(Continued).jpg)