An Ethical Dilemma Refers To A Situation Where You Must
The intensive care unit is a crucible of difficult decisions. Doctors and nurses face agonizing choices daily, weighing the sanctity of life against the realities of suffering and scarce resources. These aren't mere medical calculations; they are ethical battlegrounds where the very definition of right and wrong blurs.
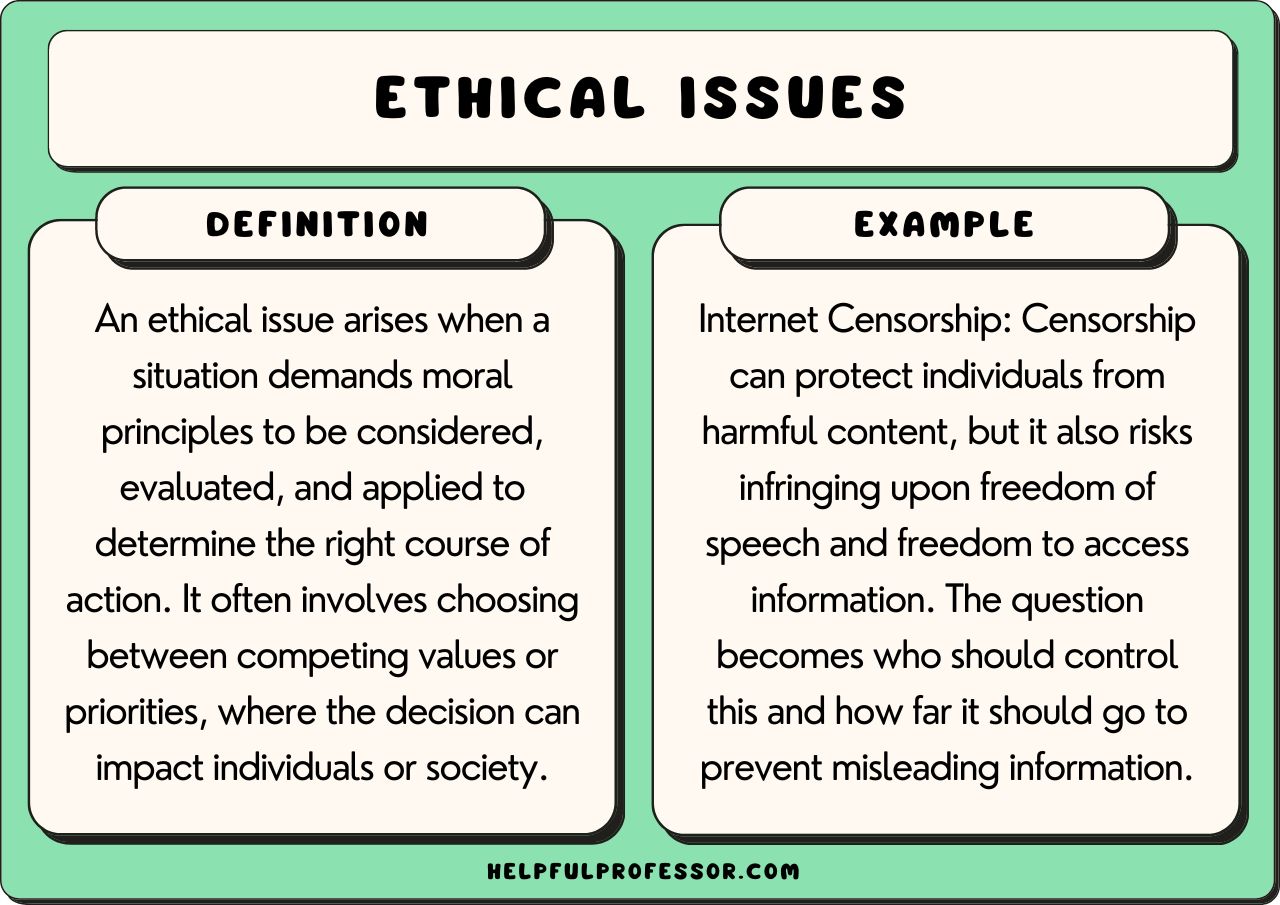
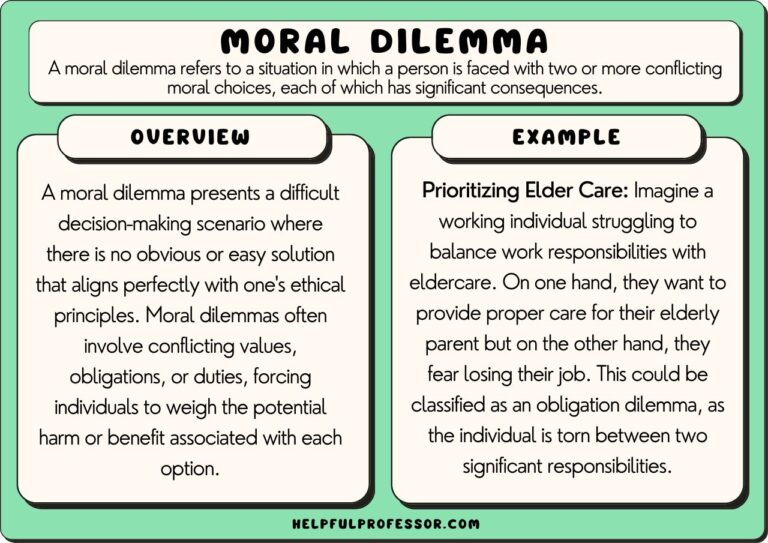
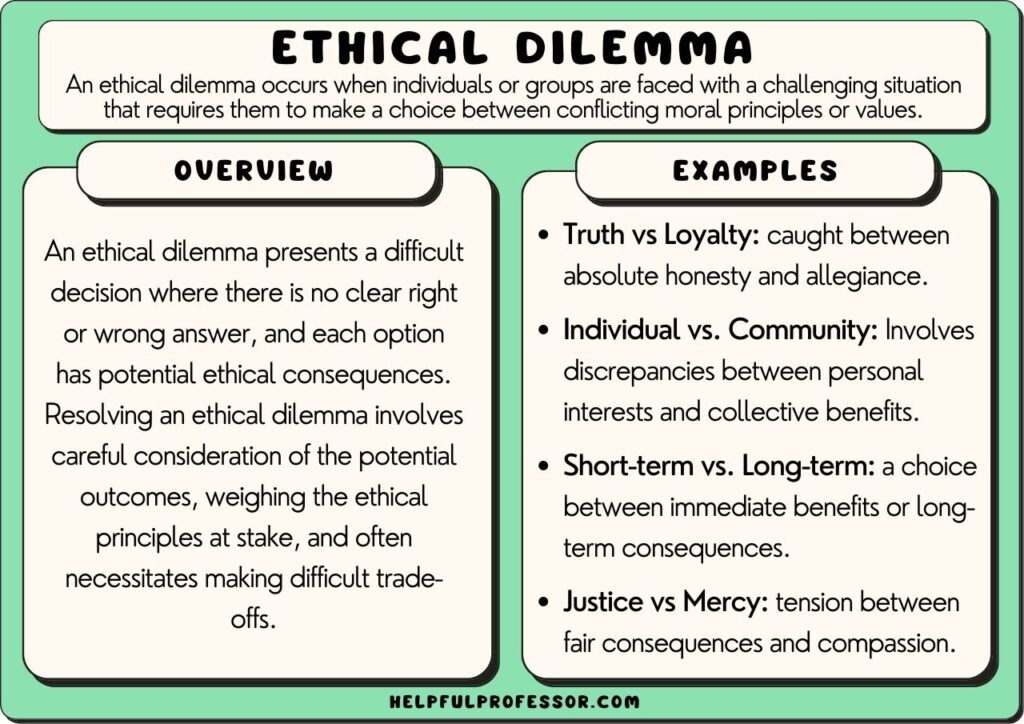
At the heart of these situations lies the ubiquitous ethical dilemma. Defined as a situation where individuals must choose between two or more conflicting ethical principles or moral imperatives, ethical dilemmas force a confrontation with our deepest values. This article explores the multifaceted nature of these dilemmas, examining their impact on healthcare professionals, patients, and society, while considering potential pathways towards resolution.
The Anatomy of an Ethical Dilemma
An ethical dilemma isn't simply a tough decision; it's a situation where any course of action violates at least one deeply held moral principle. Consider the case of a patient with a terminal illness who is suffering greatly. Should a physician administer a potentially life-shortening dose of pain medication to alleviate the suffering, even if it hastens death? This pits the principle of beneficence (doing good) against the principle of non-maleficence (doing no harm).
According to the Markkula Center for Applied Ethics at Santa Clara University, a true ethical dilemma involves a conflict between options that are all, in some sense, morally right or morally justifiable. This distinguishes it from a simple choice between right and wrong, where the morally correct course of action is clear.
Common Ethical Dilemmas in Healthcare
The landscape of healthcare is rife with situations that present ethical challenges. Resource allocation, especially in times of crisis like a pandemic, is a prime example. When ventilators are scarce, who receives priority? Age, pre-existing conditions, or potential for recovery all become factors in a heart-wrenching calculation.
Informed consent is another fertile ground for ethical dilemmas. A patient may have the right to refuse treatment, but what if that refusal is based on misinformation or a diminished mental capacity? Balancing patient autonomy with the physician's duty to protect the patient's well-being can be agonizing.
End-of-life care presents a complex web of ethical considerations. Decisions about withdrawing or withholding life-sustaining treatment, managing pain, and respecting a patient's wishes all carry significant moral weight.
The Impact on Healthcare Professionals
Facing ethical dilemmas takes a profound toll on healthcare professionals. The emotional burden of making life-altering decisions can lead to burnout, moral distress, and even post-traumatic stress disorder. The Journal of Medical Ethics has published numerous studies detailing the psychological impact of these experiences.
Nurses, often at the forefront of patient care, frequently bear the brunt of these dilemmas. They must navigate complex relationships with patients, families, and physicians, all while adhering to professional codes of conduct. The stress of these situations can significantly impact their well-being and job satisfaction.
Physicians, too, grapple with the weight of their decisions. They must balance their Hippocratic Oath with the practical realities of limited resources and the complexities of individual patient cases. The pressure to make the "right" choice can be immense.
Perspectives on Resolution
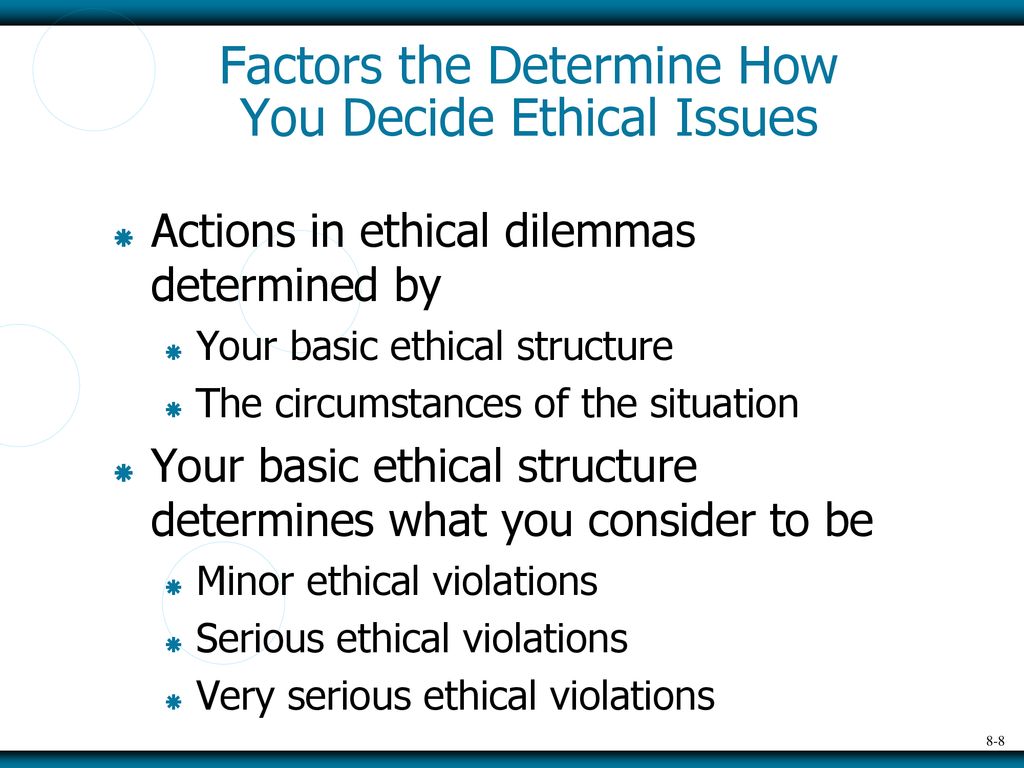
There's no single answer to resolving ethical dilemmas. A variety of approaches, from ethical frameworks to institutional ethics committees, are employed to guide decision-making. These approaches aim to provide a structured and transparent process for navigating difficult situations.
Ethical frameworks, such as utilitarianism (maximizing overall good) and deontology (following moral duties), offer different lenses through which to view a dilemma. Utilitarianism may justify prioritizing resources for those with the greatest chance of survival during a pandemic, while deontology may emphasize the inherent value of each individual life, regardless of prognosis.
Ethics committees, often found in hospitals and other healthcare institutions, provide a forum for discussing complex ethical cases. These committees typically include physicians, nurses, ethicists, and community members, offering a diverse range of perspectives.
Open communication and shared decision-making are also crucial. Engaging patients and their families in honest conversations about treatment options, risks, and benefits can help ensure that decisions align with their values and wishes. Respecting patient autonomy is paramount, even when it conflicts with medical recommendations.
Looking Ahead
As medical technology advances and healthcare systems face increasing pressures, ethical dilemmas will only become more prevalent. Artificial intelligence, genetic engineering, and resource scarcity all pose new and complex ethical challenges.
Preparing healthcare professionals to navigate these challenges is essential. Ethics education should be integrated into medical and nursing curricula, providing future clinicians with the knowledge and skills to address complex moral issues. Institutions must also create supportive environments where healthcare professionals feel empowered to raise ethical concerns and participate in ethical decision-making.
Ultimately, resolving ethical dilemmas requires a commitment to empathy, compassion, and a willingness to engage in difficult conversations. It demands a recognition that there are no easy answers and that the best course of action may involve trade-offs and compromises. By embracing ethical frameworks, fostering open communication, and supporting healthcare professionals, we can strive to navigate these complex situations with integrity and compassion.