Autologous Vs Allogeneic Stem Cell Transplant

The stakes are high for patients facing life-threatening blood cancers and immune disorders: the choice between autologous and allogeneic stem cell transplants can be life-altering. Survival rates, risks of complications, and long-term quality of life hinge on this critical decision, making understanding the nuances of each procedure paramount.
This article cuts through the medical jargon to deliver the essential facts about autologous versus allogeneic stem cell transplantation: what they are, who benefits most from each, and the critical differences that impact patient outcomes.
Understanding Stem Cell Transplantation
Stem cell transplantation is a procedure that replaces damaged or diseased blood-forming stem cells with healthy ones. These healthy cells can then grow and produce new, healthy blood cells.
There are two main types: autologous, using the patient's own stem cells, and allogeneic, using stem cells from a donor.
Autologous Stem Cell Transplantation
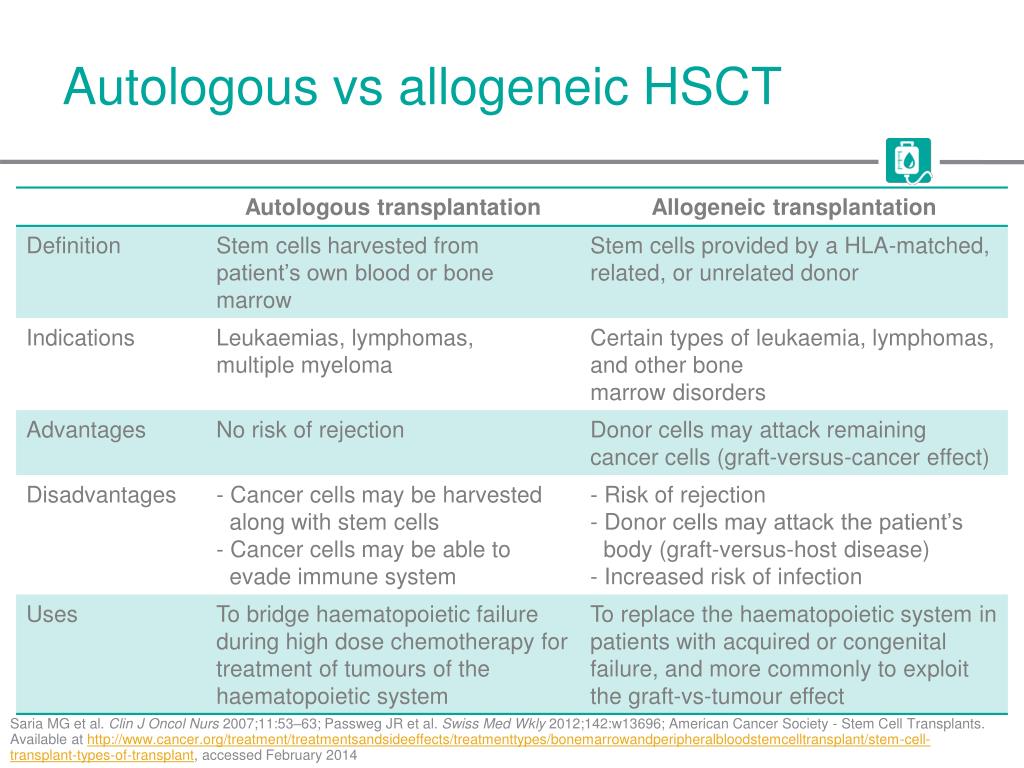
In autologous transplantation, a patient's own stem cells are collected, stored, and then returned to them after high-dose chemotherapy or radiation. This intensive treatment aims to eliminate cancer cells, but it also destroys the patient's bone marrow.
After the high-dose treatment, the stored stem cells are infused back into the patient to rebuild their bone marrow and immune system. It’s essentially a rescue procedure, allowing for higher doses of cancer-killing treatments.
Who benefits? Generally, patients with certain types of lymphoma, multiple myeloma, and some autoimmune diseases are candidates. The advantage is that there's no risk of graft-versus-host disease (GVHD).
Allogeneic Stem Cell Transplantation
Allogeneic transplantation involves receiving stem cells from a healthy donor, who may be a related or unrelated match. This approach is often considered when the patient's own stem cells are affected by disease or when the immune system needs to be replaced.
The donor's stem cells, after being infused into the patient, not only rebuild the bone marrow but also provide a new immune system that can recognize and attack any remaining cancer cells - this is called the graft-versus-tumor effect.
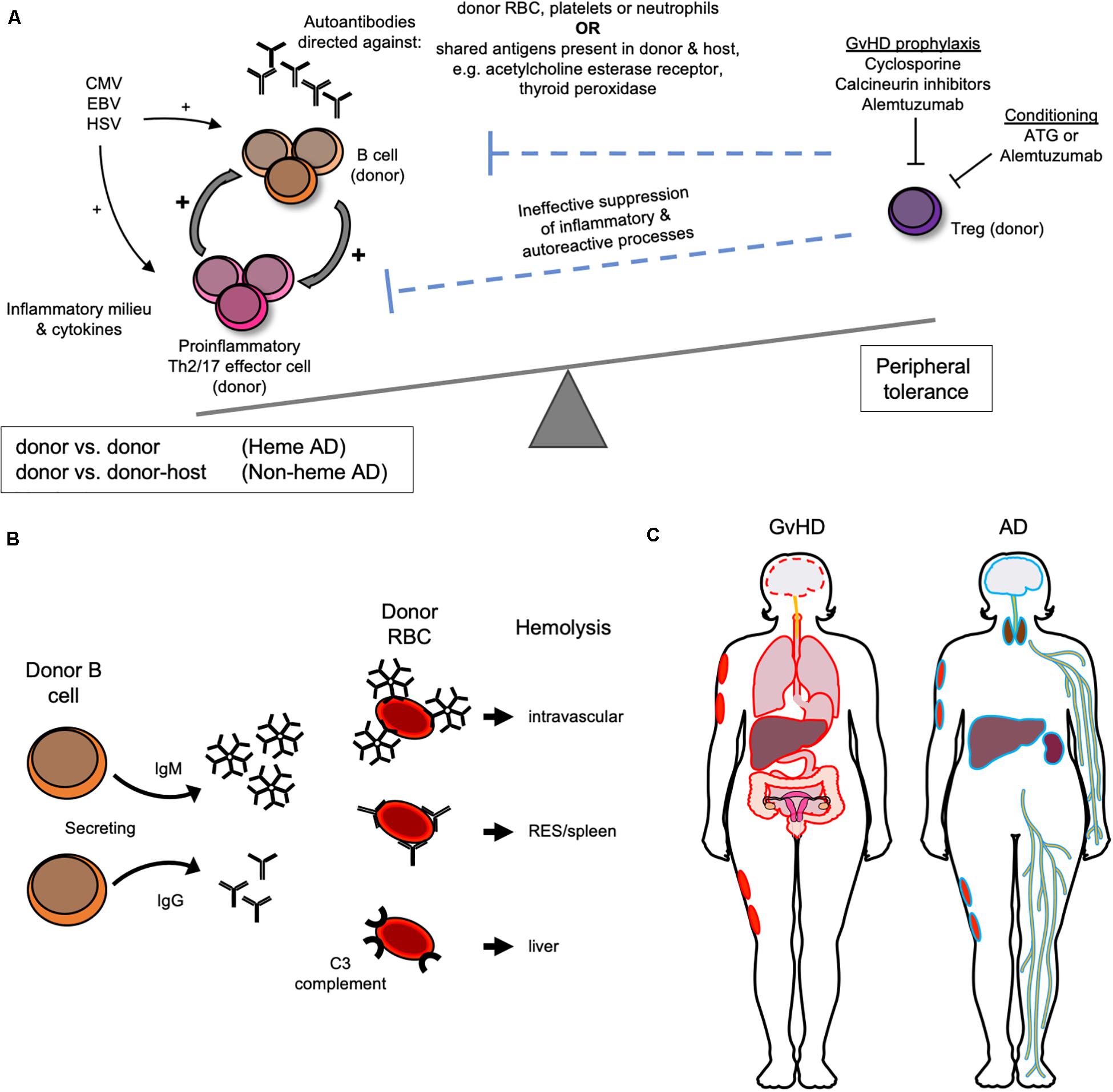
Who benefits? Patients with leukemia, myelodysplastic syndromes (MDS), aplastic anemia, and certain inherited immune deficiencies often require allogeneic transplants. The key risk is GVHD, where the donor's immune cells attack the patient's tissues.
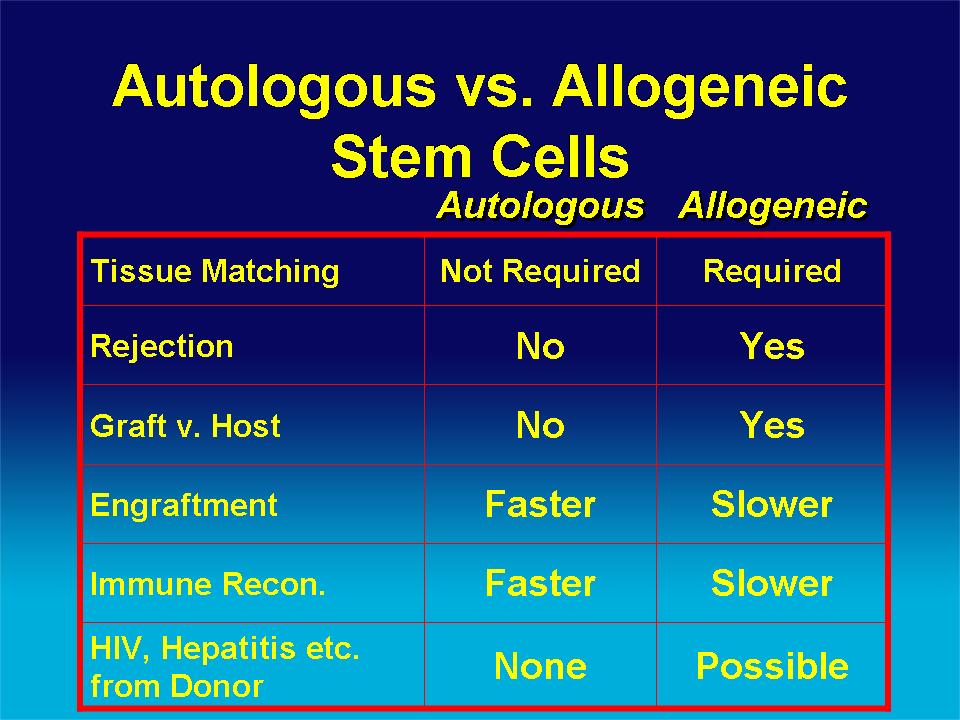
Key Differences: Autologous vs. Allogeneic
The fundamental difference lies in the source of the stem cells. Autologous uses the patient's own, while allogeneic uses a donor's.
This distinction directly impacts the risks and benefits of each procedure. Autologous eliminates GVHD but lacks the graft-versus-tumor effect; allogeneic offers the latter but carries the risk of the former.
Another crucial difference is the need for donor matching in allogeneic transplants. Human leukocyte antigen (HLA) matching is critical to minimize the risk of GVHD.
The process of finding a suitable donor can be lengthy and challenging. National registries like the Be The Match Registry play a vital role in connecting patients with unrelated donors.
Survival Rates and Outcomes
Survival rates vary significantly depending on the disease, stage, patient's overall health, and the transplant type. Data from the Center for International Blood and Marrow Transplant Research (CIBMTR) provide crucial insights.
For example, autologous transplants for multiple myeloma often show high initial response rates and prolonged remission, but relapse remains a concern. Allogeneic transplants for acute myeloid leukemia (AML) can offer a cure, but the risk of complications, including GVHD, is significant.
Long-term outcomes also differ. Autologous transplant recipients may face late effects of the high-dose chemotherapy or radiation. Allogeneic recipients need lifelong monitoring for GVHD and immune suppression.
Recent Advances and Ongoing Research
Significant advancements are improving transplant outcomes. These include better HLA matching techniques, new GVHD prevention strategies, and improved supportive care.
Haploidentical transplantation, using partially matched donors, is expanding access to allogeneic transplants for patients without fully matched donors. Post-transplant cyclophosphamide is one strategy used to reduce GVHD in haploidentical transplants.
Research is also focusing on CAR-T cell therapy, a type of immunotherapy where a patient's own immune cells are engineered to target cancer cells. This approach is showing promise for certain blood cancers, potentially impacting the role of stem cell transplantation in the future.
What’s Next?
Patients facing the decision of autologous versus allogeneic stem cell transplant must engage in thorough discussions with their medical team. This team will provide individualized risk-benefit assessments.
Continued research is essential to refine transplant techniques, improve outcomes, and expand access to these life-saving therapies. Collaboration between researchers, clinicians, and patient advocacy groups is crucial to advancing the field.
The future of stem cell transplantation holds promise for improved survival rates and quality of life for patients battling blood cancers and immune disorders.