Best Natural Supplement For Autoimmune Disease

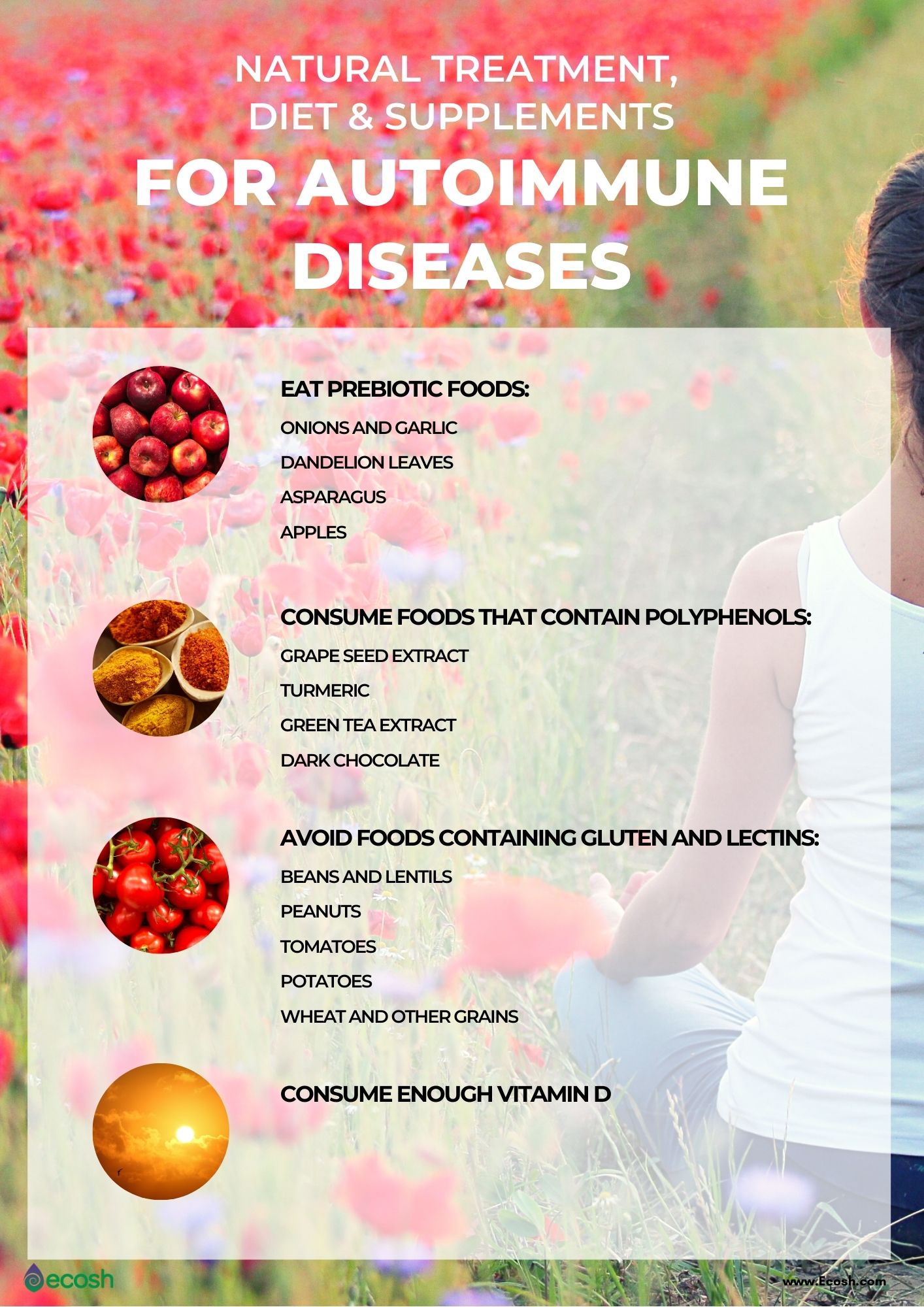
The burden of autoimmune diseases, where the body's immune system mistakenly attacks its own tissues, is immense, affecting millions worldwide. Conditions like rheumatoid arthritis, lupus, and multiple sclerosis can significantly impair quality of life. While conventional medical treatments offer relief for many, the search for complementary and alternative approaches, especially natural supplements, continues to gain momentum.
This article explores the scientific evidence surrounding natural supplements and their potential role in managing autoimmune diseases. It aims to provide an objective assessment of the current research, highlighting the promising avenues, potential limitations, and the crucial importance of consulting with healthcare professionals before incorporating any supplement into an autoimmune disease management plan. Disclaimer: This article does not provide medical advice.
The Allure of Natural Supplements
Many individuals with autoimmune diseases are drawn to natural supplements, seeking gentler or more holistic approaches to manage their symptoms. The perception is that these substances, often derived from plants or other natural sources, may offer fewer side effects compared to conventional medications.
Furthermore, some supplements are believed to address the underlying immune dysregulation characteristic of these conditions. This article investigates if this perception is based in science.
Turmeric and Curcumin: A Potent Anti-Inflammatory Duo?
Turmeric, a spice commonly used in Indian cuisine, contains curcumin, a compound known for its potent anti-inflammatory and antioxidant properties. Numerous studies have investigated curcumin's effects on various autoimmune diseases.
Research suggests that curcumin may help reduce inflammation and pain in individuals with rheumatoid arthritis. A meta-analysis published in the journal "Arthritis & Rheumatology" found that curcumin supplementation was comparable to nonsteroidal anti-inflammatory drugs (NSAIDs) in alleviating RA symptoms.
However, the bioavailability of curcumin is a significant challenge. The body doesn't readily absorb it. Formulations containing piperine (black pepper extract) or liposomal curcumin may enhance absorption, but further research is needed to determine optimal dosages and long-term efficacy.
Vitamin D: An Immune System Modulator
Vitamin D plays a crucial role in immune system regulation. Deficiency in vitamin D is prevalent in individuals with autoimmune diseases, leading researchers to explore its potential therapeutic role.
Studies have suggested that vitamin D supplementation may help modulate immune responses and reduce the severity of symptoms in conditions like multiple sclerosis and lupus. A systematic review in the "Journal of Autoimmunity" indicated a link between low vitamin D levels and increased disease activity in lupus patients.
The optimal dosage of vitamin D for individuals with autoimmune diseases remains a subject of ongoing investigation. It is essential to have vitamin D levels checked by a healthcare provider and to follow their recommendations regarding supplementation.
Omega-3 Fatty Acids: Balancing Inflammation
Omega-3 fatty acids, found in fish oil and flaxseed oil, possess anti-inflammatory properties and may help modulate immune responses. These essential fats, particularly EPA and DHA, are crucial for overall health.
Research suggests that omega-3 supplementation may benefit individuals with rheumatoid arthritis and inflammatory bowel disease (IBD). Studies have shown that omega-3s can reduce joint pain and stiffness in RA and decrease inflammation in IBD.
While generally considered safe, high doses of omega-3 fatty acids can potentially interact with blood-thinning medications. Consult with a healthcare professional before starting omega-3 supplementation, especially if you are taking other medications.
Probiotics: Gut Health and Immunity
The gut microbiome, the community of microorganisms residing in the digestive tract, plays a critical role in immune system development and regulation. Imbalances in the gut microbiome have been linked to the development and progression of autoimmune diseases.
Probiotics, live microorganisms that confer a health benefit when consumed, may help restore balance to the gut microbiome and modulate immune responses. Studies have explored the use of probiotics in managing conditions like rheumatoid arthritis and IBD.
Some research suggests that certain probiotic strains can reduce inflammation and improve gut barrier function in individuals with autoimmune diseases. However, the specific strains and dosages that are most effective remain under investigation, and the effects can vary depending on the individual and the specific autoimmune condition.
Caveats and Considerations
While natural supplements hold promise for managing autoimmune diseases, it is crucial to approach their use with caution and under the guidance of a healthcare professional. Supplements are not regulated by the FDA to the same extent as prescription medications.
Therefore, the quality and purity of supplements can vary, and interactions with other medications are possible. It's essential to buy supplements from reputable sources and to inform your doctor about any supplements you are taking.
Furthermore, it's important to recognize that supplements are not a substitute for conventional medical treatments. Autoimmune diseases are complex conditions that often require a combination of therapies, including medications, lifestyle modifications, and other interventions.
The Importance of Personalized Approach
The effectiveness of natural supplements can vary significantly from person to person. Factors such as genetics, gut microbiome composition, and overall health status can influence how an individual responds to a particular supplement.
A personalized approach, guided by a healthcare professional, is essential to determine which supplements, if any, are appropriate and safe. This approach should be based on individual needs, medical history, and potential interactions with other medications.
Looking Ahead: Future Research Directions
The field of natural supplements for autoimmune diseases is rapidly evolving. Future research should focus on conducting rigorous clinical trials to evaluate the efficacy and safety of specific supplements for various autoimmune conditions. Identifying biomarkers that can predict individual responses to supplements is also a critical area of investigation.
Furthermore, research into the gut microbiome and its role in autoimmune disease pathogenesis may lead to the development of more targeted and effective probiotic therapies. More research on bioavailability enhancers like black pepper extract or liposomal formulations of supplements is also important.
Conclusion
Natural supplements may offer potential benefits for managing autoimmune diseases, but they are not a magic bullet. While compounds like curcumin, vitamin D, and omega-3 fatty acids have shown promise in reducing inflammation and modulating immune responses, further research is needed to fully understand their efficacy and safety.
A personalized approach, guided by a healthcare professional, is crucial to determine whether supplements are appropriate and safe for each individual. It is essential to remember that supplements should complement, not replace, conventional medical treatments. Responsible and informed use of natural supplements, coupled with ongoing research, may contribute to improved outcomes for individuals living with autoimmune diseases.