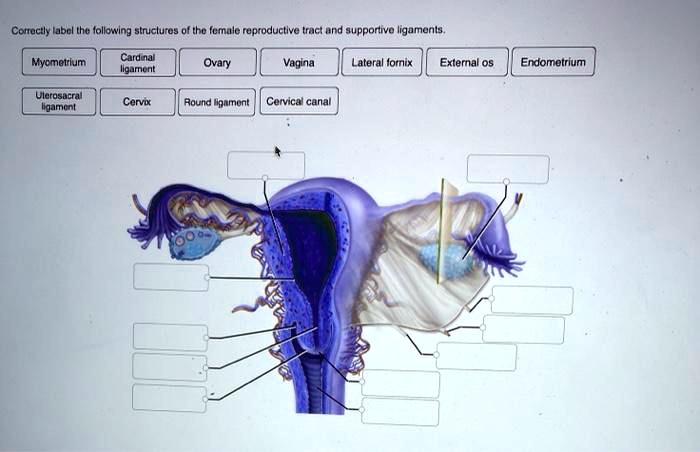
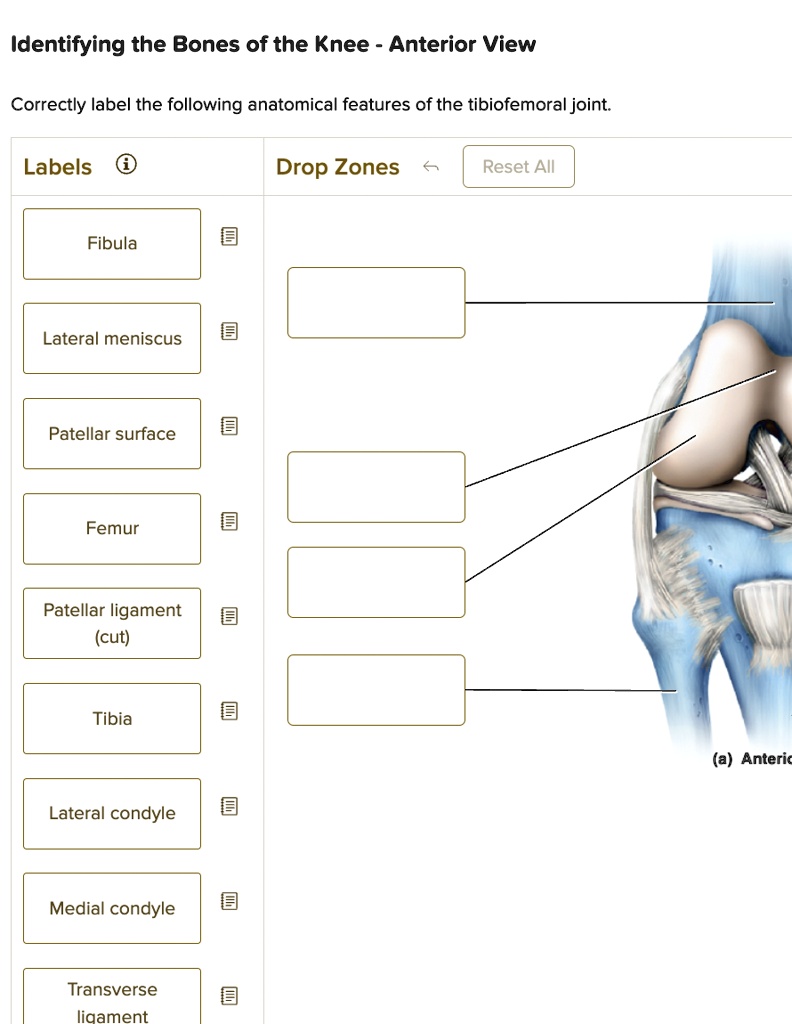
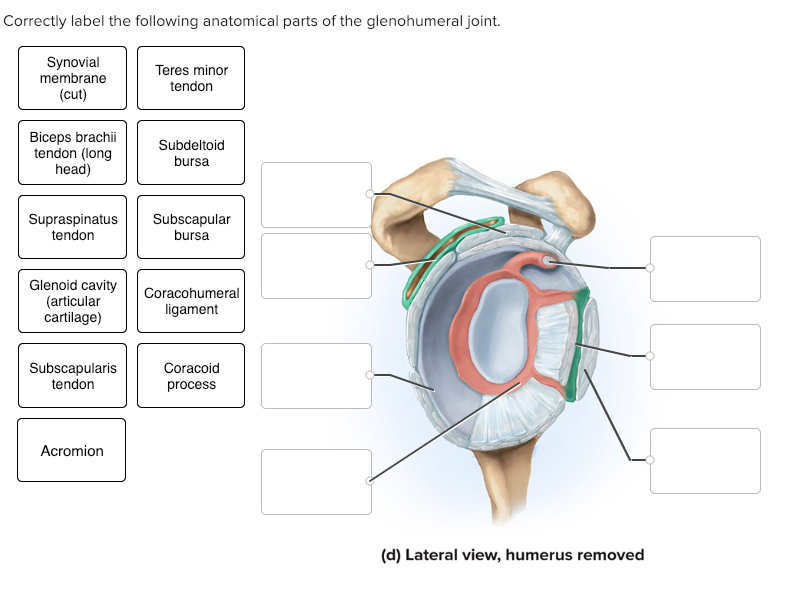
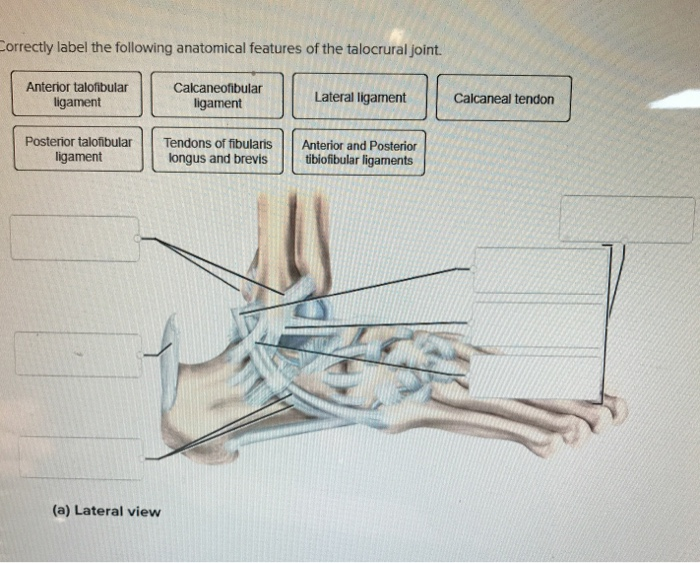
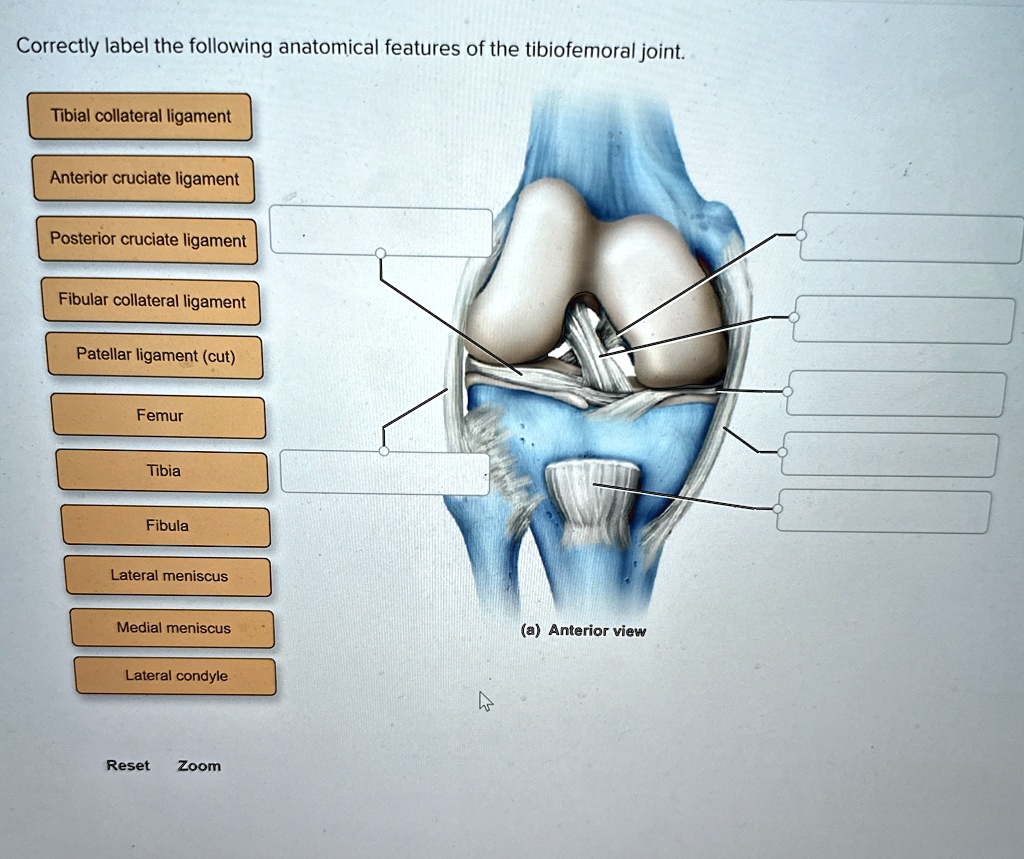
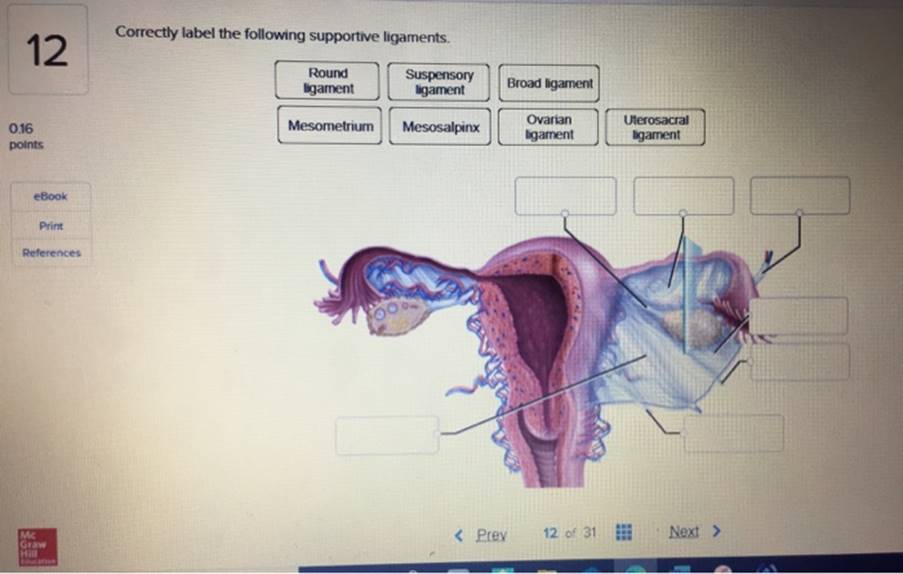
Correctly Label The Following Supportive Ligaments.
A new initiative is underway to standardize the labeling of supportive ligaments across medical education and clinical practice, aiming to reduce ambiguity and improve patient care. The project, spearheaded by a coalition of orthopedic surgeons, anatomists, and medical technology companies, seeks to address inconsistencies that have long plagued the field.
The correct and consistent identification of ligaments is crucial for accurate diagnosis, surgical planning, and effective rehabilitation. The current lack of standardization leads to confusion among medical professionals and can potentially compromise patient outcomes.
The Problem: Ambiguity in Ligament Nomenclature
The issue stems from historical variations in anatomical descriptions and the use of multiple names for the same structure. This problem is further compounded by regional differences in medical terminology, creating a significant challenge for international collaboration and knowledge sharing.
“The current system is simply not fit for purpose,” stated Dr. Emily Carter, an orthopedic surgeon and leading advocate for the initiative. “We've seen cases where surgical errors or misdiagnoses could be directly attributed to confusion over ligament identification. This initiative aims to eliminate that risk.”
The inconsistency affects everyone from medical students learning anatomy to experienced surgeons performing complex procedures. It also creates difficulties in interpreting medical imaging and research findings.
The Solution: Standardized Nomenclature and Visual Aids
The core of the initiative involves creating a comprehensive, internationally recognized standard for ligament nomenclature. This standard will be based on detailed anatomical studies and a consensus-building process involving experts from around the globe.
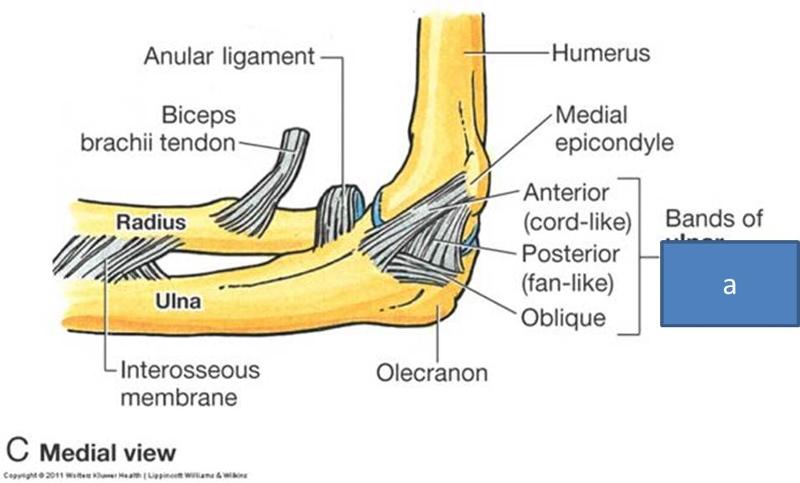
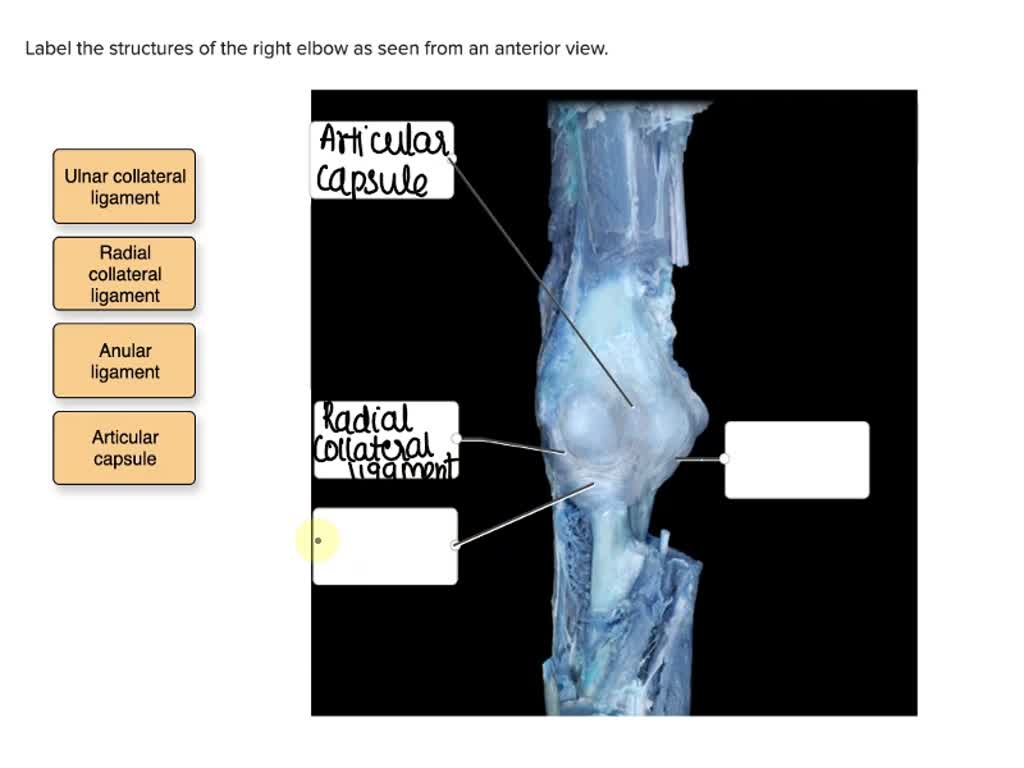
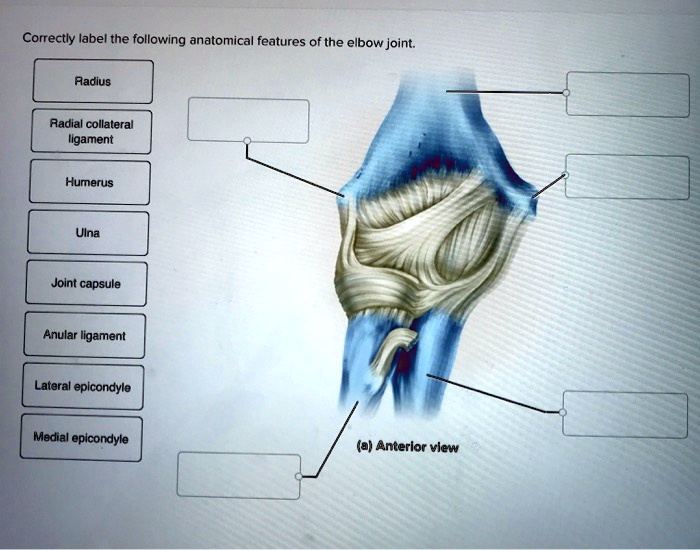
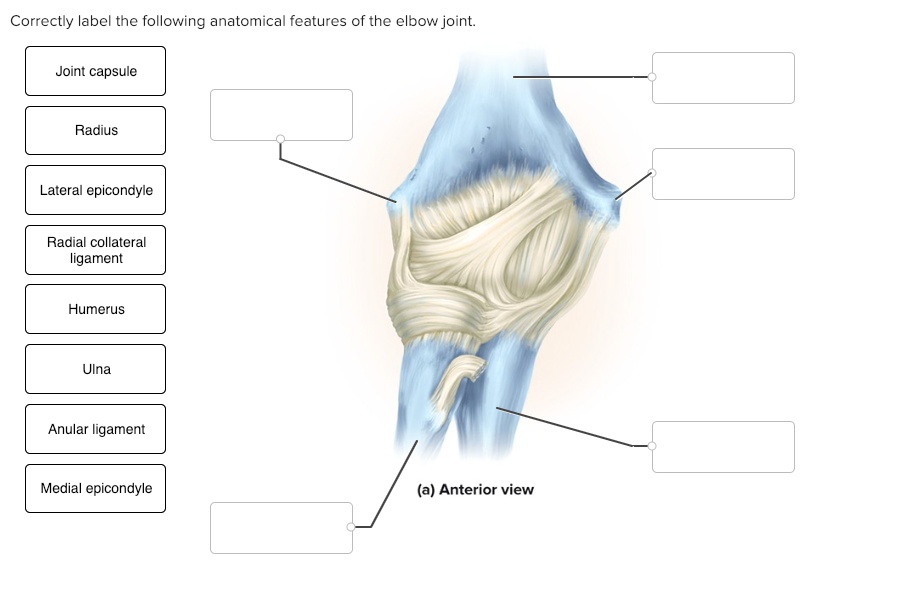
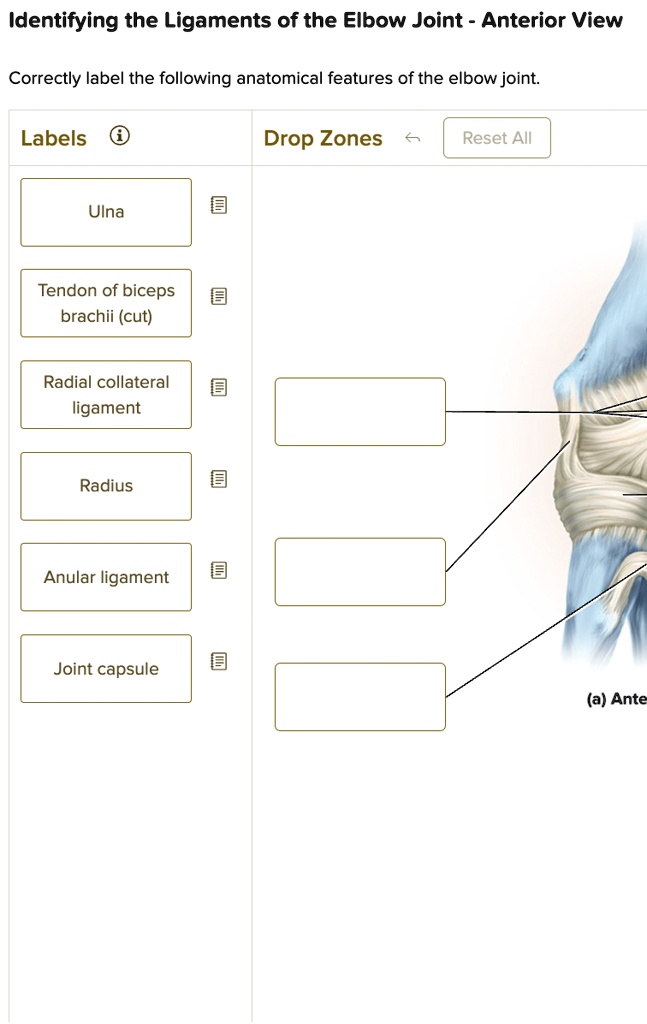
The group is also developing high-resolution anatomical illustrations and interactive 3D models to supplement the standardized nomenclature. These visual aids will be freely available to medical professionals and students through an online platform.
The proposed standard will prioritize clear, descriptive names that accurately reflect the ligament's origin, insertion, and function. Emphasis will be placed on avoiding ambiguous or potentially confusing terms.
Key Details of the Initiative
The initiative is a collaborative effort involving several key organizations, including the American Academy of Orthopaedic Surgeons (AAOS) and the International Federation of Associations of Anatomists (IFAA). Funding for the project has been secured through a combination of grants from medical research foundations and contributions from medical technology companies.
A pilot program is scheduled to begin in several medical schools and hospitals across the United States and Europe within the next six months. The results of this pilot program will be used to refine the standardized nomenclature and visual aids before widespread implementation.
The project team is actively soliciting feedback from medical professionals worldwide through online surveys and virtual workshops. This collaborative approach is essential to ensure that the final standard is both comprehensive and practical.
Potential Impact on Patient Care
The standardized nomenclature has the potential to significantly improve patient care by reducing the risk of medical errors and improving the accuracy of diagnoses. Better communication among healthcare providers will also lead to more effective treatment plans.
Improved clarity in ligament identification will also facilitate research and development of new surgical techniques and medical devices. This will ultimately lead to better outcomes for patients with musculoskeletal injuries.
"By providing a clear and consistent language for describing these critical structures, we can empower medical professionals to deliver the best possible care," said Dr. Mark Thompson, an anatomist involved in the project.
Challenges and Future Directions
One of the main challenges will be overcoming resistance to change within the medical community. Some physicians may be reluctant to adopt new terminology after years of using familiar, albeit inconsistent, names.
However, the project team is confident that the benefits of standardization will ultimately outweigh any initial inconvenience. They are planning a comprehensive outreach campaign to educate medical professionals about the new standard and its advantages.
Future directions for the initiative include developing standardized protocols for medical imaging and surgical documentation. These protocols will further enhance the consistency and accuracy of ligament identification in clinical practice.
The successful implementation of this initiative could serve as a model for other areas of medicine where inconsistent terminology poses a challenge. Standardizing nomenclature is a crucial step towards improving communication and ensuring patient safety.
A Human-Interest Perspective
For patients like Sarah Miller, a young athlete who suffered a knee injury, the initiative offers hope for a more streamlined and accurate diagnosis. "I was so confused by all the different terms the doctors were using," she said. "It made me feel like they weren't even talking about the same thing. A standardized system would give me more confidence in my treatment."
Stories like Sarah's highlight the real-world impact of this initiative and the importance of clear communication in healthcare. The initiative isn't just about standardizing names; it's about improving lives.
The move to correctly and consistently label supportive ligaments represents a significant step forward in medical practice. By fostering clearer communication and reducing ambiguity, this initiative has the potential to improve patient outcomes and advance the field of musculoskeletal medicine. This will positively impact how new generations learn and how experts share ideas.