Does Lung Transplant Cure Cystic Fibrosis

The sterile air hummed with the quiet efficiency of a hospital ward. Sunlight streamed through the window, illuminating dust motes dancing in the air, a stark contrast to the unseen battle raging within young Liam's lungs. For years, Cystic Fibrosis (CF) had relentlessly tightened its grip, each breath a labored effort. Now, a lung transplant offered a chance at a life previously unimaginable—a life filled with unburdened laughter, spontaneous adventures, and the simple joy of breathing easy.
This raises a crucial question for the CF community: Does a lung transplant actually cure Cystic Fibrosis? The answer, while filled with hope, is nuanced. While a lung transplant dramatically improves quality of life and extends lifespan for many with advanced CF, it is not a cure. The underlying genetic defect that causes CF remains, impacting other organs and requiring ongoing management.
Understanding Cystic Fibrosis
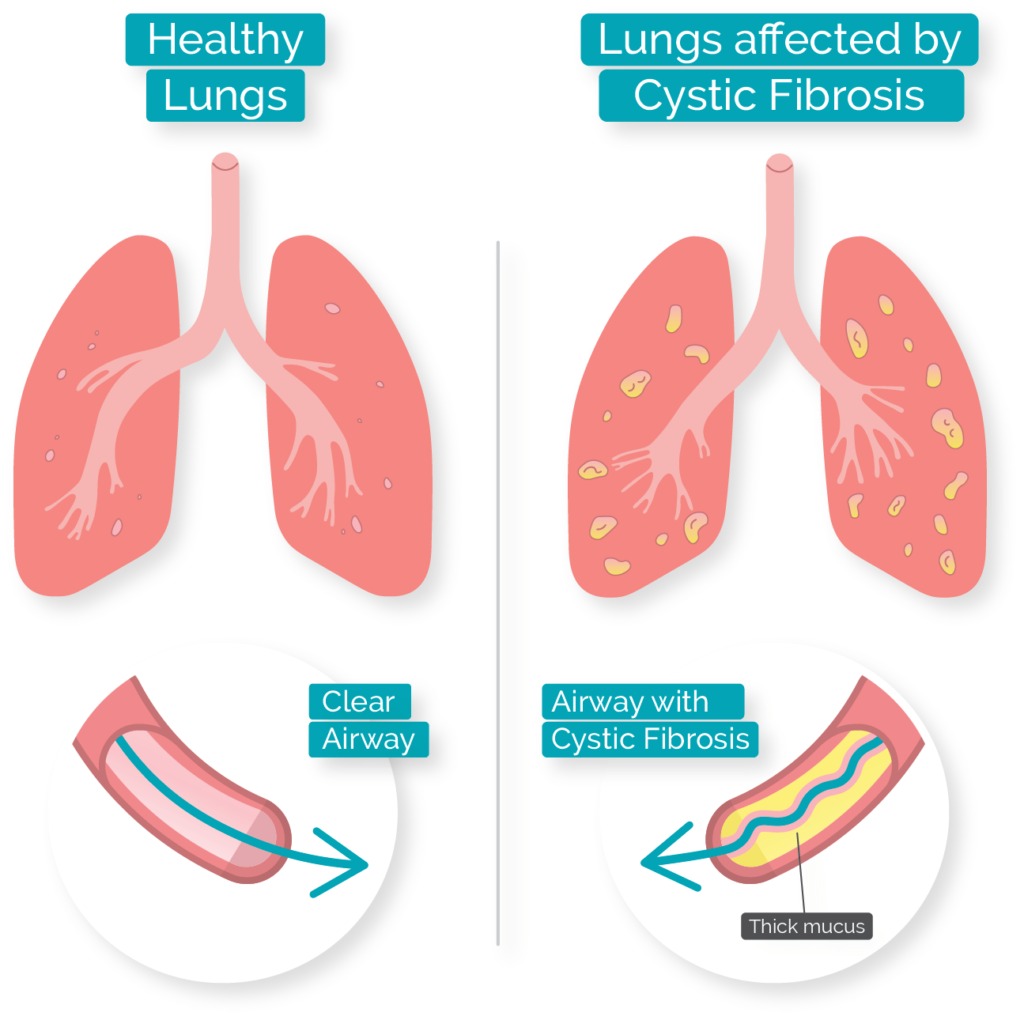
CF is a genetic disorder affecting the lungs, pancreas, liver, intestines, sinuses, and reproductive organs. It’s caused by a defective gene that leads to the production of thick, sticky mucus.
This mucus clogs the airways in the lungs, making it difficult to breathe and creating a breeding ground for bacteria, leading to chronic infections and progressive lung damage. Over time, this damage becomes irreversible, making everyday activities a struggle.
The Cystic Fibrosis Foundation (CFF) has been instrumental in funding research and developing therapies to manage CF. Their efforts have significantly improved the lives of individuals with CF, extending life expectancy and enhancing quality of life.
The Promise of Lung Transplantation
For individuals with end-stage lung disease due to CF, lung transplantation can be a life-saving option. When lung function deteriorates to the point where it severely impacts daily life and medical management becomes increasingly difficult, a transplant may be considered.
During a lung transplant, the diseased lungs are replaced with healthy lungs from a deceased donor. This immediately alleviates the breathing difficulties caused by CF-damaged lungs.
Recipients often experience a dramatic improvement in their ability to breathe, exercise, and participate in daily activities. The hope is to regain a quality of life lost to the progression of the disease.
Why Lung Transplant Isn't a Cure
While transplanted lungs are free of CF, the underlying genetic mutation persists throughout the recipient's body. This means that other organs affected by CF remain susceptible to its effects.
According to the National Institutes of Health (NIH), individuals who undergo lung transplantation for CF may still experience complications related to CF in other parts of their body, such as pancreatic insufficiency or diabetes.
Moreover, transplant recipients must take immunosuppressant medications for the rest of their lives to prevent their body from rejecting the new lungs. These medications can have significant side effects, including increased risk of infection, kidney problems, and certain types of cancer.
Continued Management After Transplant
Even with healthy lungs, individuals who have undergone lung transplantation for CF still require ongoing medical care. This includes regular monitoring for complications, managing other CF-related health issues, and adhering to a strict medication regimen.
The Mayo Clinic emphasizes the importance of a multidisciplinary approach to post-transplant care. This involves a team of specialists, including pulmonologists, transplant surgeons, nurses, and therapists, working together to optimize the patient's health.
Dietary management is also crucial, as many CF patients experience pancreatic insufficiency and require enzyme supplementation to properly digest food. Furthermore, regular exercise and pulmonary rehabilitation can help maintain lung function and overall fitness.
Improved Outcomes and Life Expectancy
Despite the challenges, lung transplantation has significantly improved outcomes for individuals with end-stage lung disease due to CF. Studies have shown that lung transplant recipients generally live longer and have a better quality of life than those who remain on medical management alone.
Data from the Organ Procurement and Transplantation Network (OPTN) shows that survival rates after lung transplantation for CF have steadily improved over the years.
Although there are risks involved, the potential benefits of lung transplantation for carefully selected candidates are substantial, offering a chance to live a fuller, more active life.
The Future of CF Treatment
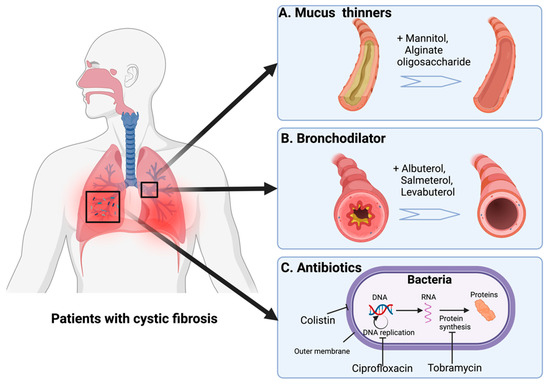
While lung transplantation remains an important option for those with advanced CF, the focus is increasingly shifting towards therapies that address the underlying genetic defect. Groundbreaking medications known as CFTR modulators are revolutionizing CF treatment.
These drugs target the defective CFTR protein, helping it to function more effectively and reducing the production of thick mucus. For many individuals with specific CFTR mutations, these medications can significantly improve lung function and reduce the need for lung transplantation.
The development of CFTR modulators represents a major breakthrough in CF treatment, offering hope for a future where lung transplantation may become less common. Research continues to explore new and improved therapies, including gene editing and other innovative approaches.
“The advancements in CF treatment are truly remarkable. We are seeing incredible progress in our ability to manage this disease and improve the lives of those affected. While lung transplantation remains an important option, the future of CF treatment is incredibly bright." – Dr. Emily Carter, Pulmonologist.
A Life-Changing Procedure, Not a Cure
Lung transplantation for CF is a complex and life-altering procedure. It offers a new lease on life by replacing diseased lungs with healthy ones.
However, it's essential to understand that it is not a cure for Cystic Fibrosis. The genetic defect remains, requiring ongoing management of other affected organs and lifelong immunosuppression.
The ultimate goal remains to find a cure for CF that addresses the underlying genetic cause. Until that day arrives, lung transplantation will continue to play a vital role in extending and improving the lives of individuals with advanced CF.
Liam's Story Continues
Liam, now several years post-transplant, is living proof of the transformative power of this procedure. He runs, he plays, he breathes freely—activities that were once unimaginable.
He still diligently takes his medications and attends regular check-ups, understanding the ongoing management required. He also actively participates in the CF community, sharing his story and offering hope to others.
Liam's journey highlights the complex realities of living with CF and the profound impact that lung transplantation can have. It reminds us that while a cure remains the ultimate goal, the strides made in treatment and care offer a brighter future for those living with this challenging disease.










:max_bytes(150000):strip_icc()/understanding-cystic-fibrosis-998213_fin-f6b10f0a2a474ba08c40907fff1556dc.png)