During The Primary Assessment Circulation Is Evaluated By Assessing

In emergency medical care, the seconds following a traumatic event or sudden illness can be the difference between life and death. While advanced interventions often dominate the narrative, the bedrock of effective emergency response lies in a systematic and rapid primary assessment. This assessment, a cornerstone of medical protocols worldwide, centers around identifying and addressing immediate threats to life, with circulation taking a prominent position.
The vital importance of assessing circulation during the primary assessment cannot be overstated. The nut graf is that a properly functioning circulatory system ensures adequate oxygen and nutrient delivery to vital organs, a function that is catastrophically compromised during events like severe bleeding, cardiac arrest, or shock. This assessment determines whether the heart is pumping effectively, if blood vessels are intact, and if blood is circulating adequately to maintain organ viability, making it one of the most critical steps in stabilizing a patient and dictating immediate treatment strategies.
The ABCs of Primary Assessment: C Stands for Circulation
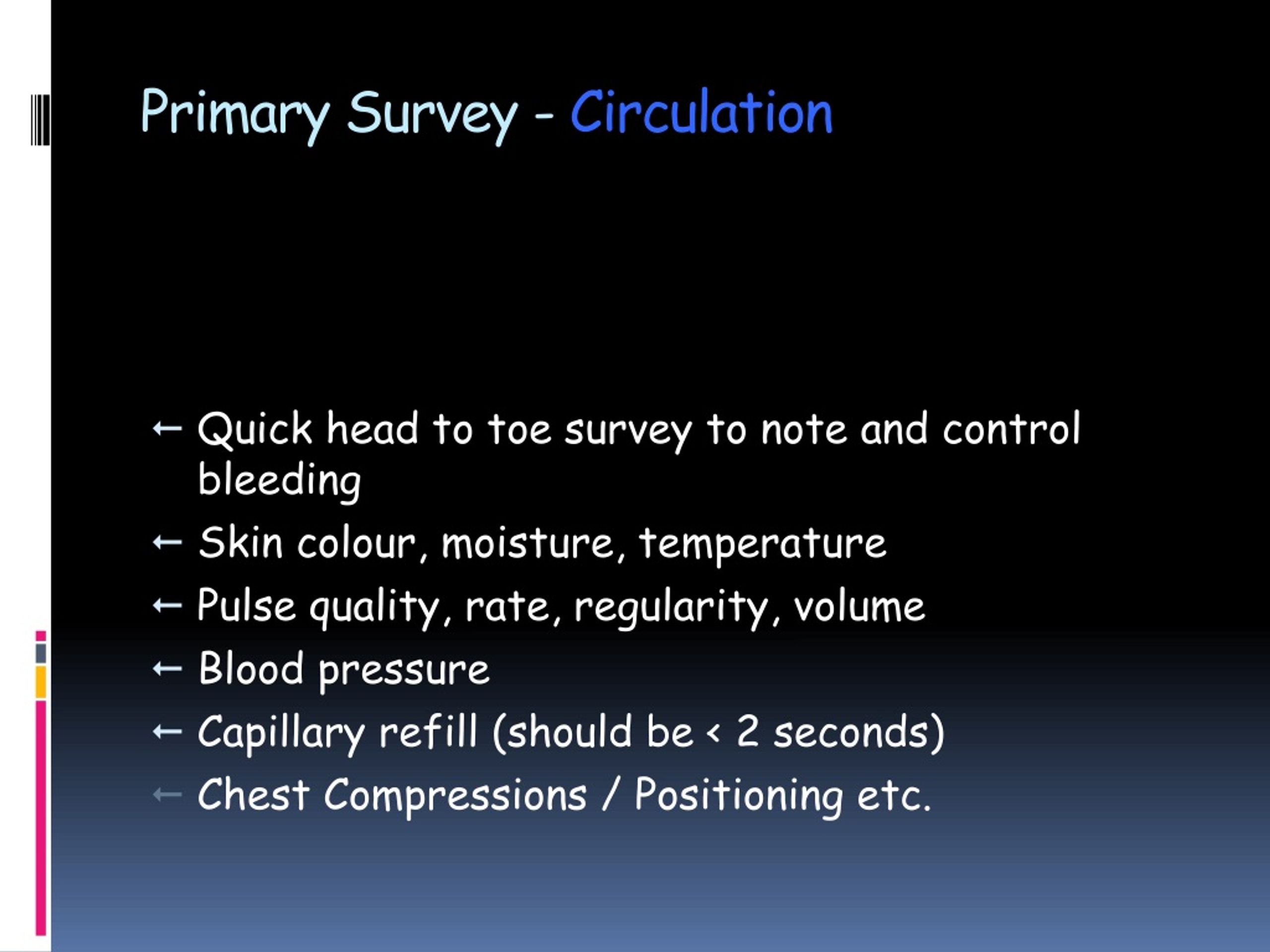
The primary assessment typically follows the ABCDE mnemonic: Airway, Breathing, Circulation, Disability, and Exposure. Circulation, the 'C' in this crucial sequence, focuses on evaluating the efficacy of the cardiovascular system. Its objective is to quickly detect signs of inadequate perfusion and initiate appropriate interventions.
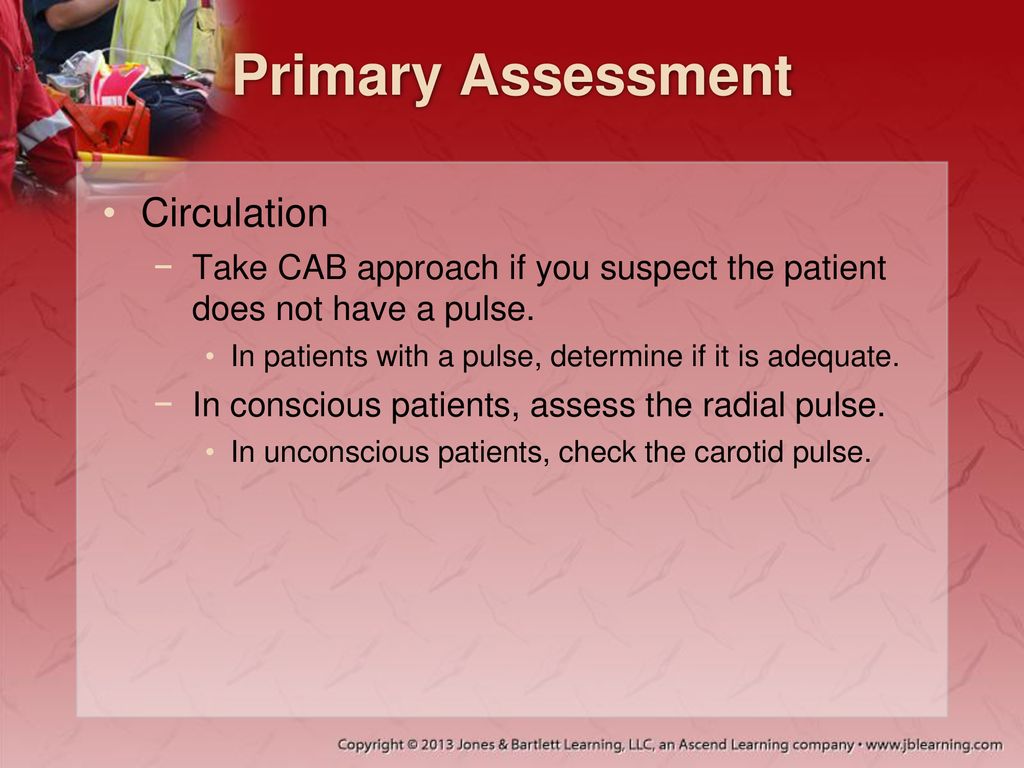
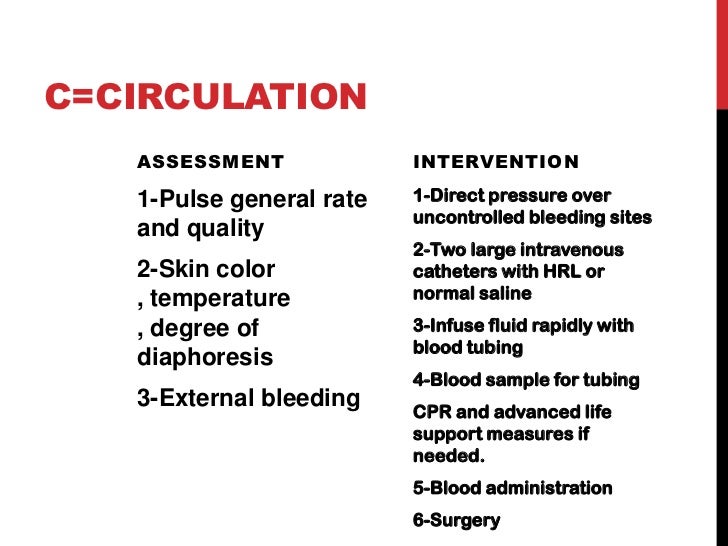
One of the initial steps in assessing circulation is checking for a pulse. The presence, rate, and quality of the pulse provide valuable information. A rapid, weak pulse can indicate hypovolemia (low blood volume) due to hemorrhage or dehydration, while a slow pulse might suggest bradycardia or certain medication effects.
Conversely, an absent pulse necessitates immediate action, usually cardiopulmonary resuscitation (CPR). This emphasizes the critical role circulation plays in prioritizing interventions.
Key Indicators: Pulse, Skin, and Capillary Refill
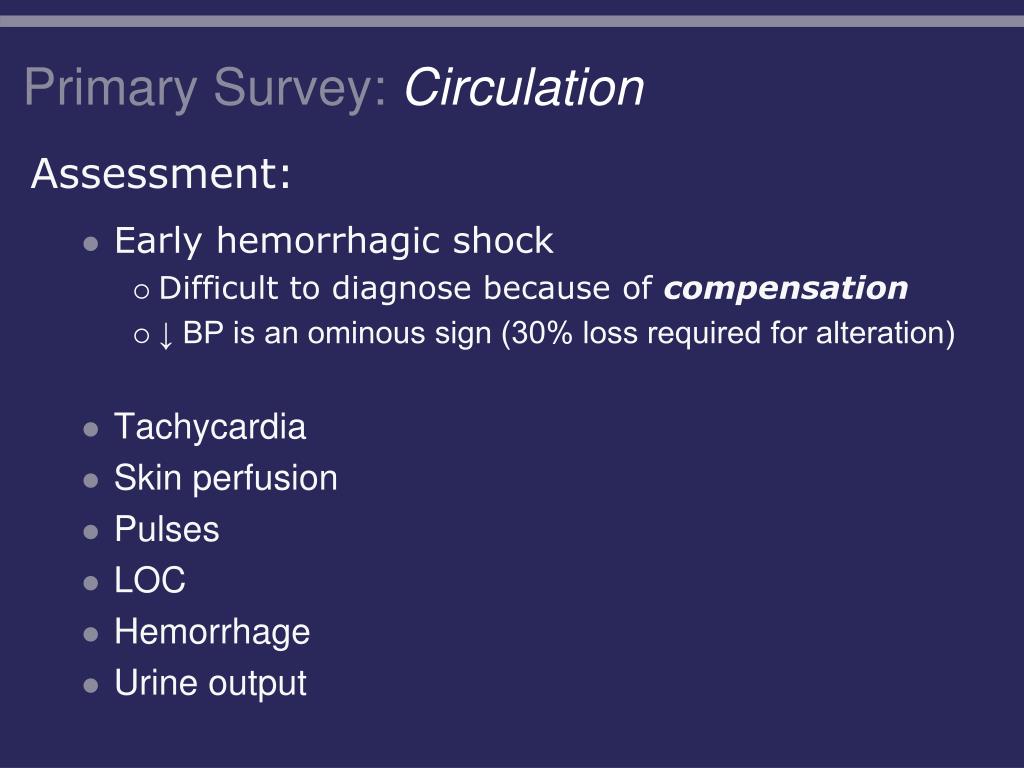
Beyond pulse assessment, the evaluation extends to skin condition. Cool, clammy, and pale skin suggests poor perfusion, often associated with shock or vasoconstriction. This is in stark contrast to warm, dry skin, which indicates more stable circulatory status.
Capillary refill time (CRT) is another simple yet informative assessment. This involves pressing on a fingernail or toenail until it blanches, then releasing and observing how quickly the color returns. A prolonged CRT (typically more than two seconds) often suggests inadequate peripheral perfusion.
It is important to note that CRT may be less reliable in cold environments or in patients with certain pre-existing conditions.
Beyond the Basics: Advanced Circulation Assessment
While pulse, skin, and CRT form the cornerstone of initial circulation assessment, more advanced techniques may be employed in pre-hospital settings or emergency departments. These are especially beneficial when dealing with complex cases.
Non-invasive blood pressure monitoring provides a quantitative measure of circulatory function. Hypotension (low blood pressure) is a common sign of circulatory compromise and often necessitates fluid resuscitation or vasopressor administration.
Invasive monitoring, such as arterial lines, provides continuous blood pressure readings and allows for frequent blood sampling. These are typically reserved for critically ill patients requiring intensive care.
The Role of Technology: Point-of-Care Testing
Point-of-care testing (POCT) has revolutionized emergency medicine, enabling rapid assessment of key circulatory parameters. Lactate levels, for instance, can indicate the degree of tissue hypoxia, a consequence of inadequate perfusion.
Arterial blood gas (ABG) analysis provides information about oxygenation, carbon dioxide levels, and pH, all of which are closely linked to circulatory function. These tests aid in guiding treatment decisions and monitoring patient response to therapy.
Challenges and Future Directions
Assessing circulation during the primary assessment is not without its challenges. Factors such as environmental conditions, patient age, and pre-existing medical conditions can complicate the evaluation. Obesity, for example, can make it difficult to palpate pulses accurately.
Ongoing research focuses on developing more accurate and non-invasive methods for assessing circulation. Techniques such as near-infrared spectroscopy (NIRS) show promise in monitoring tissue oxygenation in real-time.
Artificial intelligence (AI) and machine learning are also being explored to enhance the accuracy and efficiency of circulation assessment. AI-powered algorithms could analyze multiple physiological parameters to identify subtle signs of circulatory compromise earlier than human clinicians.
The Importance of Training and Teamwork
Effective circulation assessment requires rigorous training and adherence to standardized protocols. Emergency medical technicians (EMTs), paramedics, and physicians all receive extensive training in these techniques.
Teamwork is also essential. A coordinated approach, with clear communication and delegation of tasks, ensures that circulation is assessed quickly and efficiently. Simulation training plays a vital role in preparing healthcare professionals for real-world emergencies.
Regular refresher courses and continuing medical education are crucial to maintain proficiency in circulation assessment and stay abreast of new developments.
Conclusion: Protecting the Lifeline
The assessment of circulation during the primary assessment remains a cornerstone of emergency medical care. By swiftly identifying and addressing circulatory compromise, healthcare professionals can significantly improve patient outcomes.
Continued innovation in assessment techniques, coupled with rigorous training and collaborative teamwork, will further refine this critical aspect of emergency response. Ultimately, the goal is to protect the lifeline of every patient, ensuring that vital organs receive the oxygen and nutrients they need to survive and thrive. Prioritizing circulation is not merely a step in a process; it is a commitment to safeguarding life itself.







.jpg)


.jpg)