Fluid Electrolyte Imbalance Nursing Care Plan

The critical role of nurses in managing fluid and electrolyte imbalances is gaining increased attention as healthcare systems grapple with aging populations and complex medical conditions. These imbalances, potentially life-threatening, require meticulous monitoring, precise intervention, and a comprehensive nursing care plan. This article delves into the core components of such care plans, emphasizing the practical application of nursing knowledge in restoring and maintaining patient homeostasis.
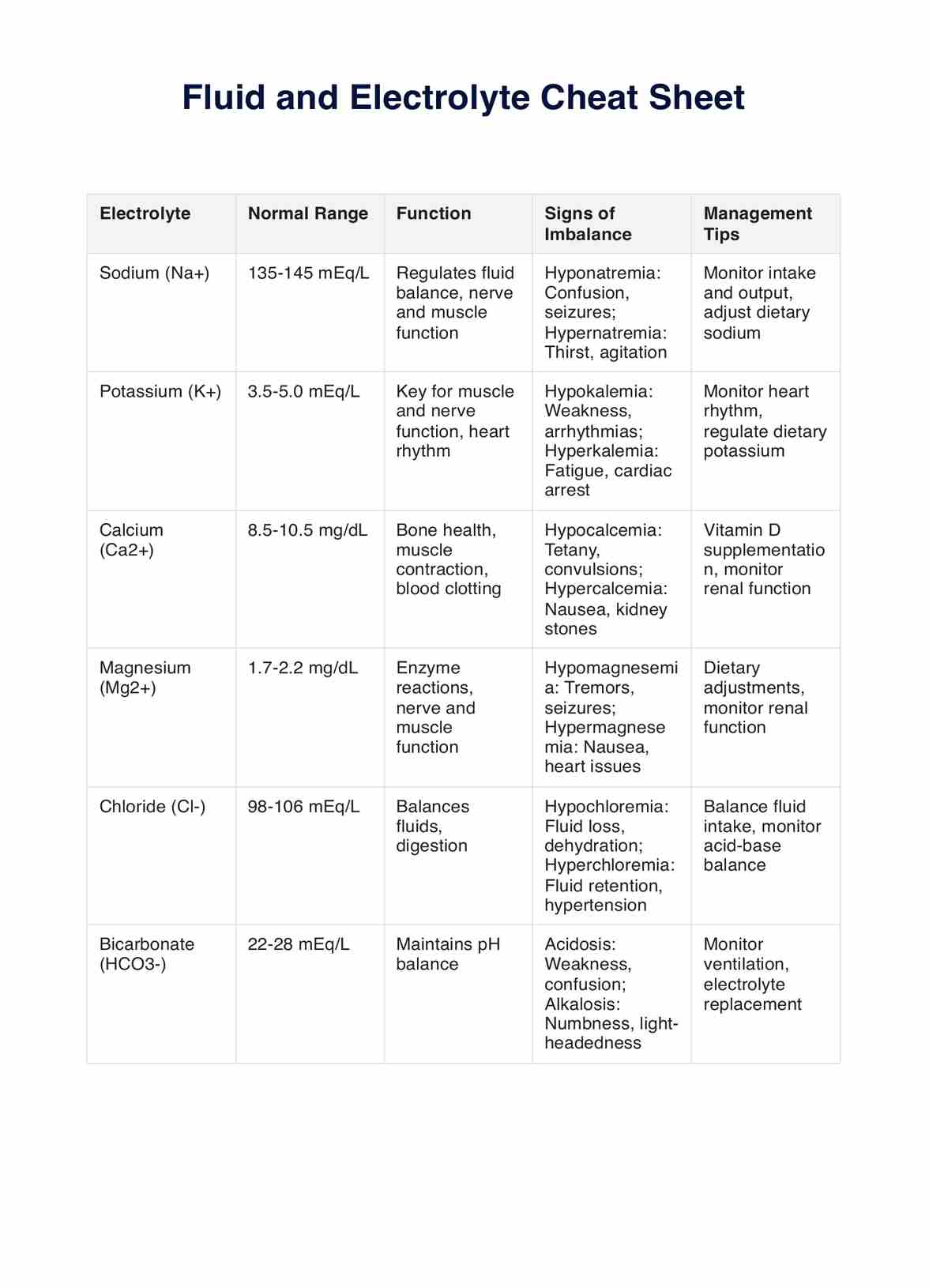
Fluid and electrolyte imbalances occur when the body's fluid volume or the levels of essential minerals like sodium, potassium, calcium, and magnesium deviate from their normal ranges. These imbalances can result from a wide variety of conditions, including dehydration, overhydration, kidney disease, heart failure, and certain medications. Effective nursing care is essential for early detection, accurate assessment, and tailored interventions to prevent complications.
Assessment: The Foundation of the Care Plan
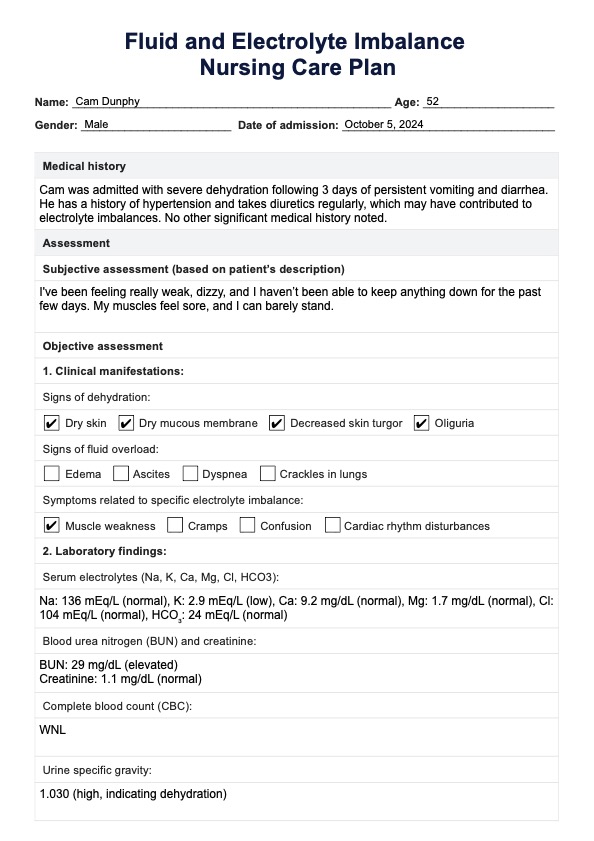
The first step in developing a nursing care plan for fluid and electrolyte imbalance is a thorough assessment. This involves collecting data through various methods, including patient history, physical examination, and review of laboratory results.
Patient history should encompass details about existing medical conditions, medication use (especially diuretics and corticosteroids), dietary habits, and recent fluid intake and output. Any reports of nausea, vomiting, diarrhea, muscle weakness, or confusion should be carefully documented.
Physical examination includes assessing vital signs (heart rate, blood pressure, respiratory rate, temperature), skin turgor, mucous membranes, edema, and neurological status. Auscultation of lung sounds can reveal signs of fluid overload, while palpation of peripheral pulses assesses circulation.
Laboratory results provide crucial objective data. Key values to monitor include serum electrolytes (sodium, potassium, chloride, bicarbonate, calcium, magnesium, phosphate), blood urea nitrogen (BUN), creatinine, serum osmolality, urine specific gravity, and arterial blood gases (ABGs).
Nursing Diagnoses: Identifying the Problem
Based on the assessment findings, the nurse formulates one or more relevant nursing diagnoses. Common diagnoses associated with fluid and electrolyte imbalances include: Fluid Volume Deficit, Fluid Volume Excess, Risk for Electrolyte Imbalance, and Impaired Gas Exchange.
Each diagnosis should be clearly defined and supported by evidence from the assessment data. For example, a patient exhibiting signs of dehydration, such as poor skin turgor, concentrated urine, and elevated serum sodium, might receive the diagnosis of Fluid Volume Deficit.
Planning and Implementation: Tailored Interventions
The planning phase involves setting specific, measurable, achievable, relevant, and time-bound (SMART) goals for patient outcomes. These goals guide the selection and implementation of nursing interventions.
Fluid Management
For Fluid Volume Deficit, the primary goal is to restore fluid balance. This may involve administering oral fluids, intravenous (IV) fluids, or a combination of both. The type and rate of IV fluid administration must be carefully prescribed by a physician and closely monitored by the nurse.
For Fluid Volume Excess, the focus is on reducing fluid overload. Interventions include restricting fluid intake, administering diuretics, monitoring urine output, and elevating the patient's legs to reduce edema. In severe cases, dialysis may be necessary.
Electrolyte Management
Electrolyte imbalances require specific interventions to correct the deficiency or excess. Potassium imbalances are particularly critical, as both hyperkalemia and hypokalemia can lead to cardiac arrhythmias. Potassium replacement can be administered orally or intravenously, with careful monitoring of cardiac rhythm.
Sodium imbalances also require careful management. Hyponatremia, a low sodium level, can be treated with fluid restriction or, in severe cases, hypertonic saline. Hypernatremia, a high sodium level, typically requires fluid replacement and sodium restriction.
Monitoring and Evaluation
Continuous monitoring is essential throughout the implementation phase. This includes frequent assessment of vital signs, fluid balance, electrolyte levels, and the patient's response to interventions.
The nurse must promptly report any significant changes or adverse reactions to the physician. The effectiveness of the interventions is evaluated based on the patient's progress toward the established goals. If the goals are not being met, the care plan needs to be revised.
Patient Education: Empowering Self-Care
Patient education is a vital component of the nursing care plan. Patients need to understand the nature of their fluid and electrolyte imbalance, the importance of adhering to their treatment plan, and strategies for preventing future occurrences.
This includes education on dietary modifications, fluid intake recommendations, medication management, and recognizing early warning signs of imbalance. For example, patients with heart failure need to be educated about sodium restriction and the importance of daily weight monitoring.
The Impact on Patient Outcomes
Effective nursing care plays a crucial role in improving patient outcomes related to fluid and electrolyte imbalances. Early detection, accurate assessment, and tailored interventions can prevent complications such as cardiac arrhythmias, seizures, and organ damage.
By providing comprehensive care and education, nurses empower patients to actively participate in their own health management. This leads to improved adherence to treatment plans, reduced hospital readmissions, and enhanced quality of life.
In conclusion, the nursing care plan for fluid and electrolyte imbalances is a dynamic and essential tool for restoring and maintaining patient homeostasis. By employing a systematic approach based on thorough assessment, accurate diagnosis, tailored interventions, and comprehensive patient education, nurses can significantly improve patient outcomes and quality of life.