How Long Is Your Immune System Compromised After Chemo

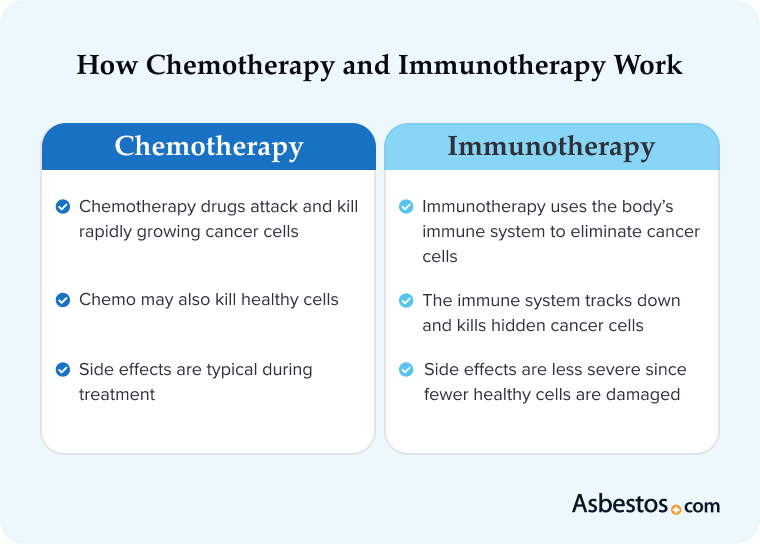
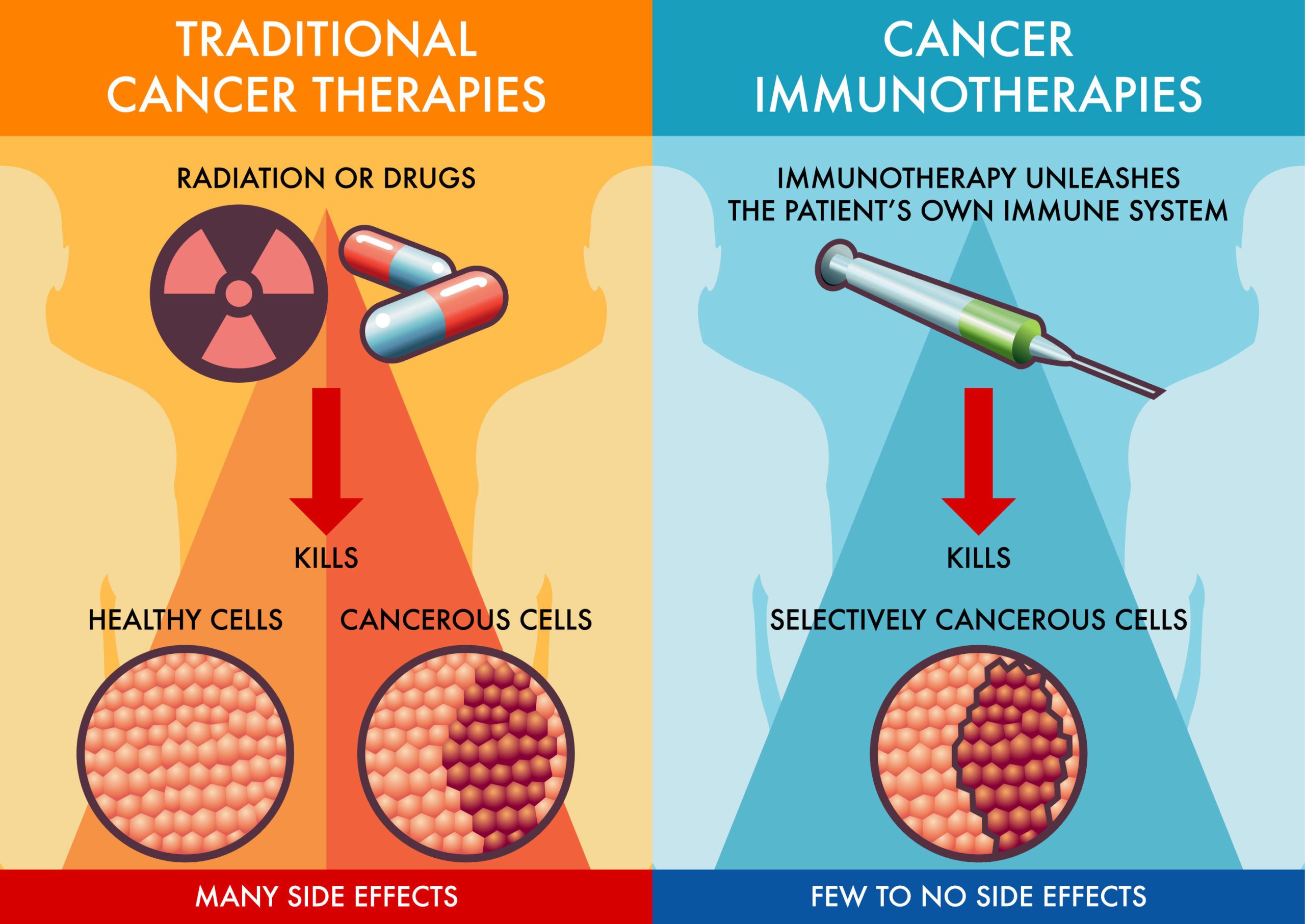
The fight against cancer often involves powerful weapons, and chemotherapy is one of the most potent. While it targets and destroys cancerous cells, it also inflicts collateral damage on the immune system, leaving patients vulnerable to infections. The question on many patients' minds is: How long will this vulnerability last?
Understanding the timeline of immune recovery after chemotherapy is crucial for both patients and healthcare providers. This knowledge allows for informed decisions about preventative measures, lifestyle adjustments, and the timing of subsequent treatments or procedures. The recovery period is not uniform, and factors such as the type of chemotherapy, the individual's overall health, and the presence of other medical conditions all play a significant role in determining the duration of immune compromise.
The Immediate Impact of Chemotherapy on the Immune System
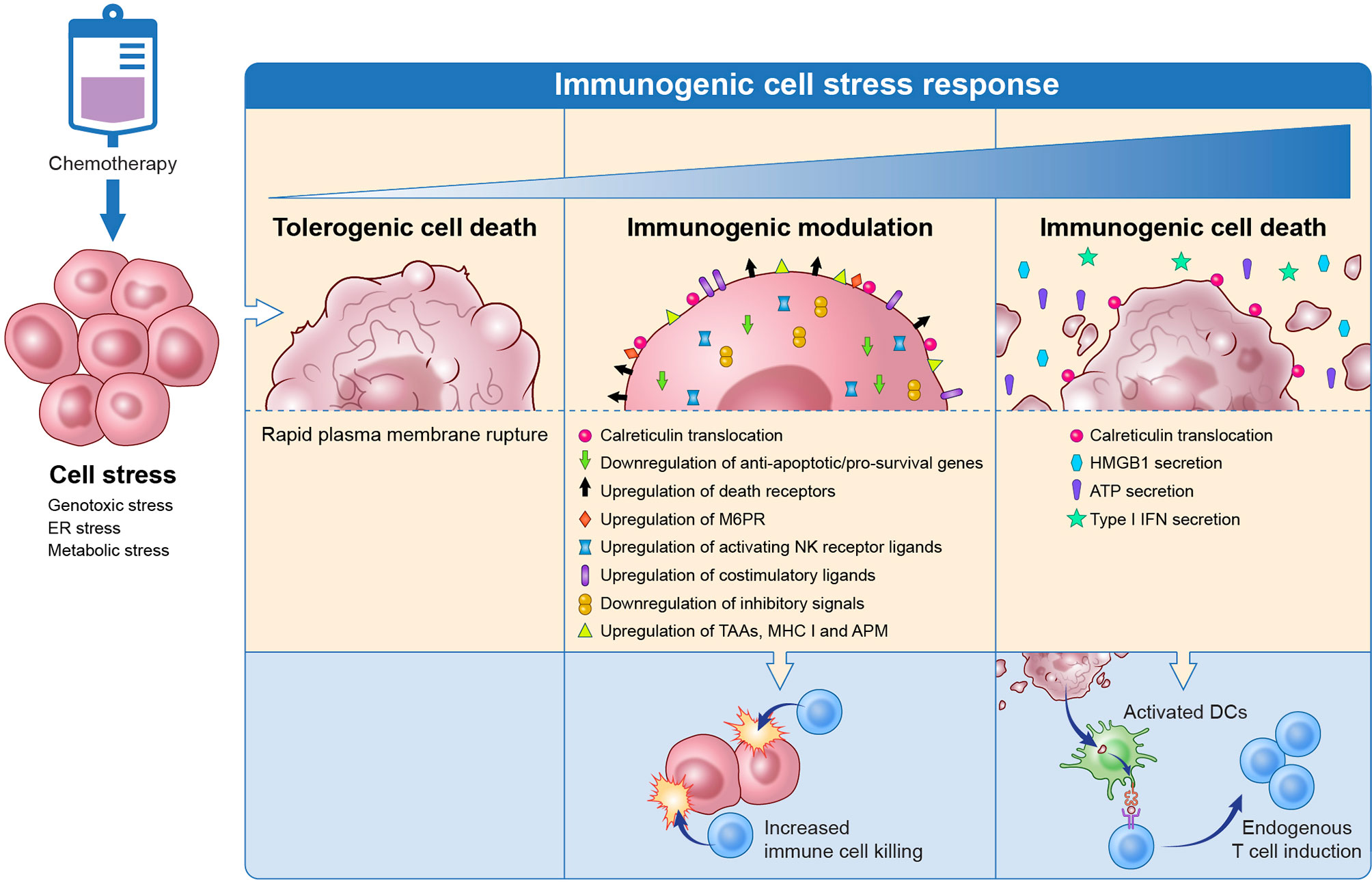
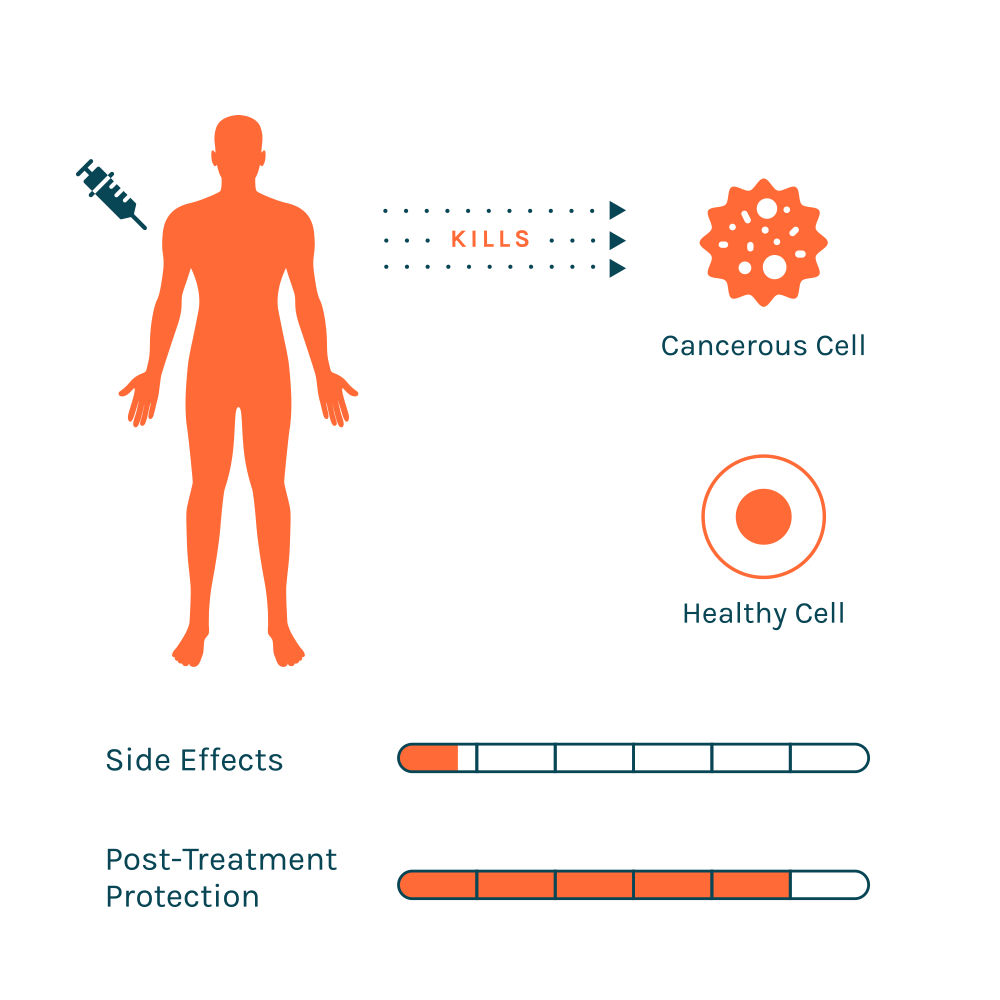
Chemotherapy drugs are designed to kill rapidly dividing cells. Unfortunately, this includes not only cancer cells but also healthy cells like those in the bone marrow, where immune cells are produced.
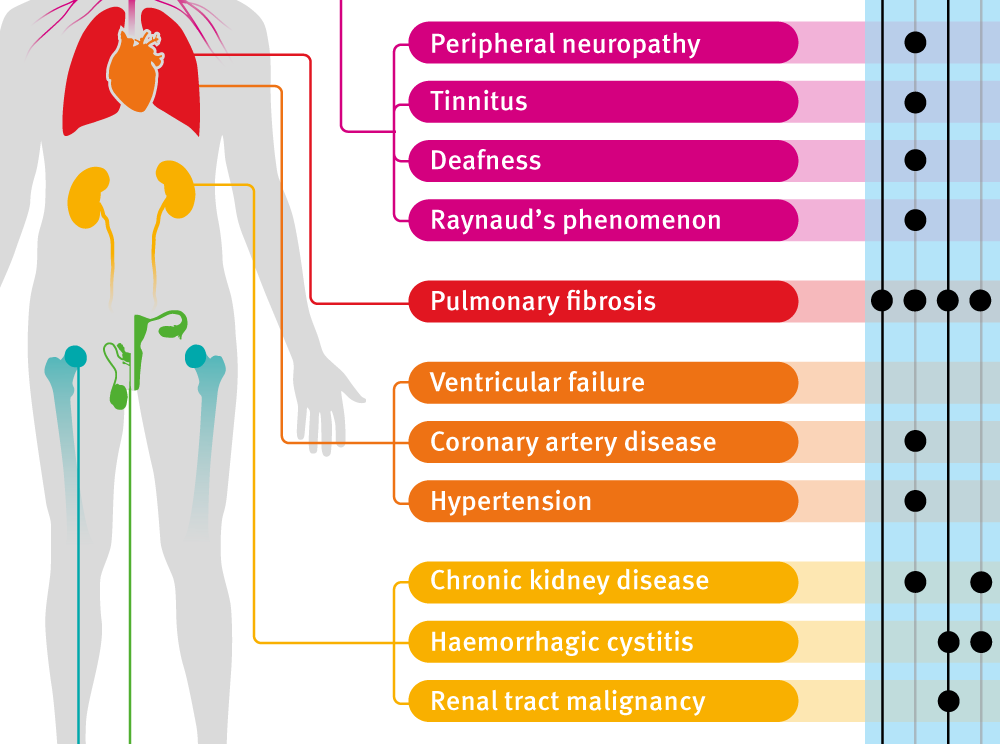
This destruction leads to myelosuppression, a condition characterized by a decrease in the production of blood cells, including white blood cells (WBCs), which are essential for fighting infections. The most critical type of WBC affected is the neutrophil, and a low neutrophil count is known as neutropenia.
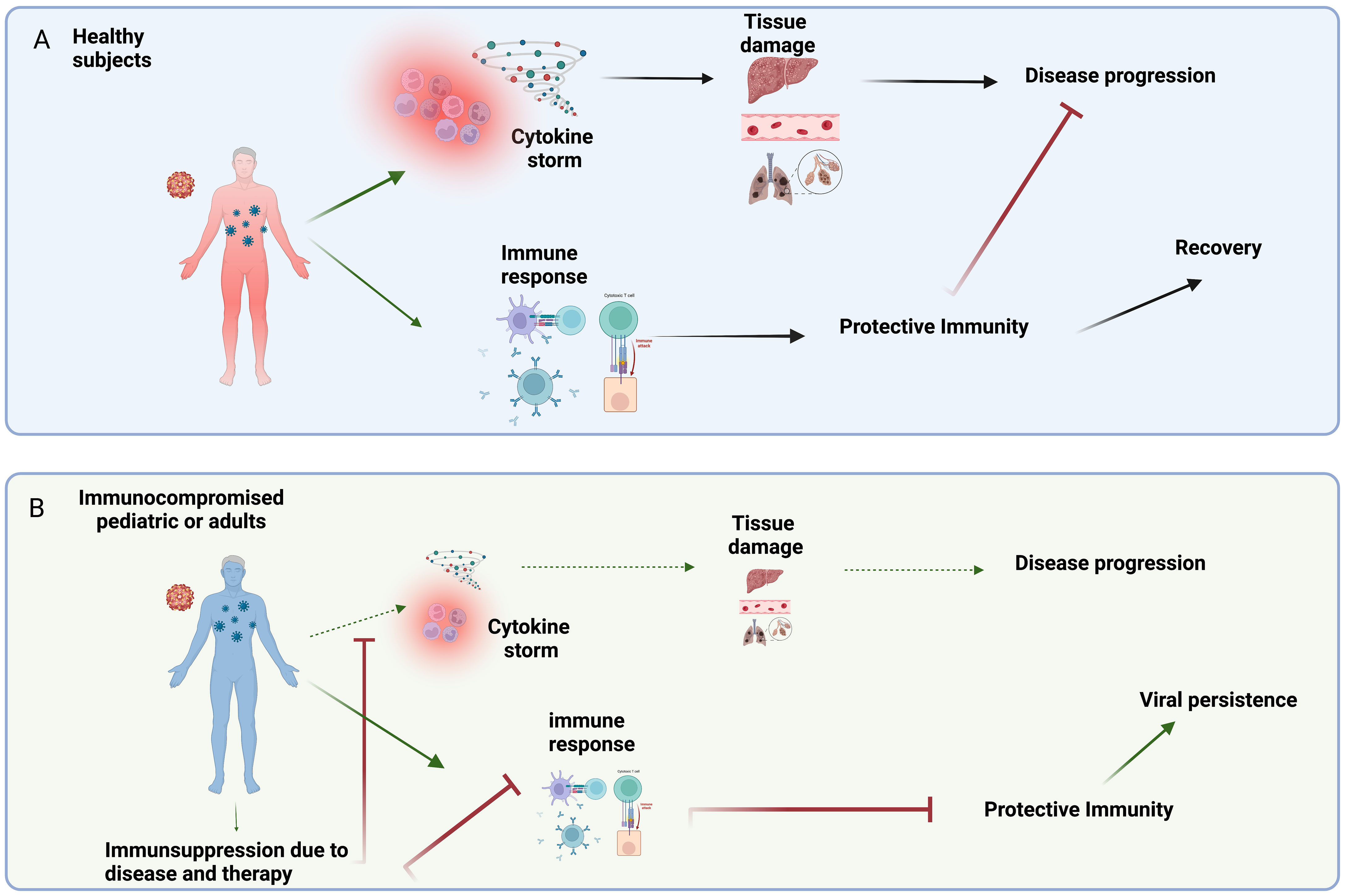
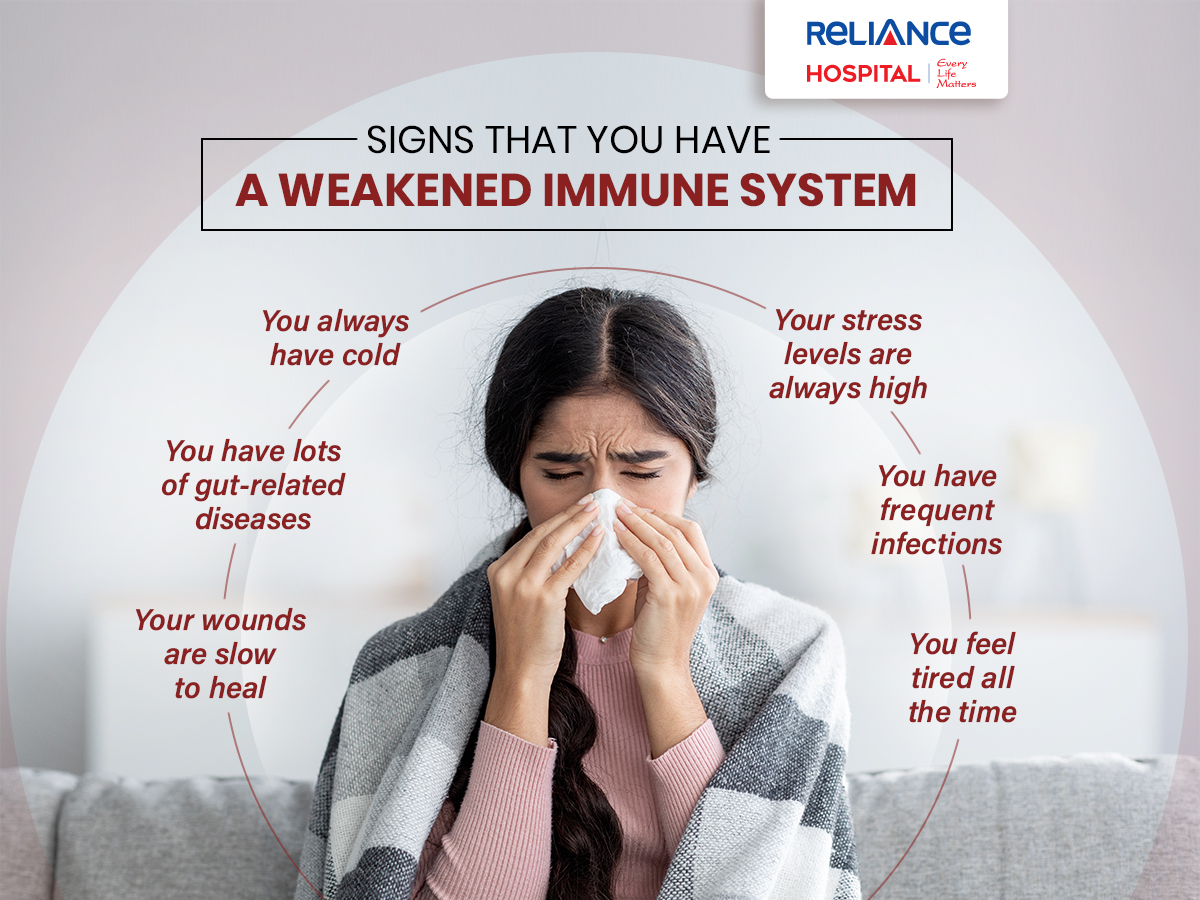
Neutropenia significantly increases the risk of infection, as the body's ability to combat bacteria, fungi, and viruses is severely compromised. Patients experiencing neutropenia are often advised to take precautions, such as avoiding crowds, practicing meticulous hygiene, and being vigilant for signs of infection like fever, chills, or cough.
The Nadir and Immediate Recovery
The point at which blood cell counts reach their lowest level after chemotherapy is called the nadir. The nadir typically occurs between 7 and 14 days after chemotherapy, but it can vary depending on the specific drugs used and the individual's response to treatment.
During the nadir, the risk of infection is at its highest. After the nadir, the bone marrow begins to recover, and blood cell counts gradually increase.
However, even as blood cell counts rise, the immune system may not be fully functional immediately. The newly produced immune cells may be immature or less effective at fighting off infections.
Long-Term Immune Recovery: A Variable Timeline
The duration of immune compromise after chemotherapy varies considerably from person to person. Several factors influence the recovery timeline.
Type of Chemotherapy
Different chemotherapy drugs have different effects on the immune system. Some drugs are more myelosuppressive than others, leading to a more profound and prolonged decrease in blood cell counts. High-dose chemotherapy regimens, often used in preparation for stem cell transplants, can cause severe and prolonged immune suppression.
The specific combination of drugs used in a chemotherapy regimen also affects the immune recovery. Regimens that include drugs known to be particularly toxic to the bone marrow will likely result in a longer period of immune compromise.
Individual Health and Prior Treatments
A patient's overall health status prior to chemotherapy plays a significant role in how quickly their immune system recovers. Patients with pre-existing conditions, such as diabetes or autoimmune diseases, may experience slower immune recovery.
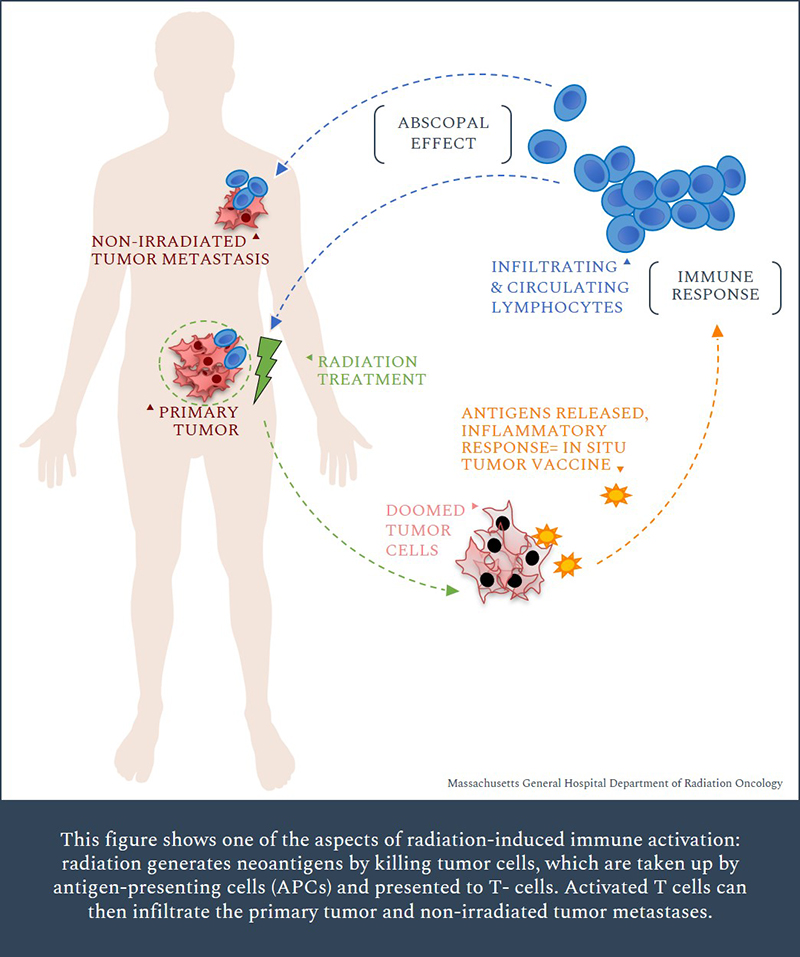
Previous treatments, including prior chemotherapy or radiation therapy, can also impact immune function and potentially prolong the recovery period. The cumulative effect of multiple treatments can weaken the bone marrow's ability to produce new blood cells.
Age
Age is a significant factor in immune recovery. Older adults tend to have a less robust immune system to begin with, and their bone marrow may not be as efficient at producing new blood cells after chemotherapy.
As a result, older patients may experience a more prolonged period of immune compromise and be at higher risk of infections. They may also take longer to respond to vaccinations, which are often recommended after chemotherapy to restore immunity against vaccine-preventable diseases.
Monitoring and Management of Immune Compromise
Regular monitoring of blood cell counts is essential during and after chemotherapy. This allows healthcare providers to assess the degree of myelosuppression and adjust treatment plans as needed.
Growth factors, such as granulocyte colony-stimulating factor (G-CSF), can be used to stimulate the bone marrow to produce more neutrophils. These medications can help shorten the duration of neutropenia and reduce the risk of infection.
Preventative measures are crucial for managing immune compromise. These include practicing good hygiene, avoiding contact with sick people, and being vigilant for signs of infection.
"The goal is to minimize the risk of infection during the period of immune vulnerability," explains Dr. Anya Sharma, an oncologist specializing in hematologic malignancies. "This often involves a combination of medication, lifestyle modifications, and close monitoring."
Vaccination After Chemotherapy
Vaccination is an important strategy for restoring immunity against vaccine-preventable diseases after chemotherapy. However, the timing of vaccination is critical. Live vaccines, such as the measles, mumps, and rubella (MMR) vaccine, are generally contraindicated in immunocompromised patients.
Inactivated vaccines, such as the influenza and pneumococcal vaccines, can be given, but their effectiveness may be reduced if the immune system is still significantly compromised. Healthcare providers typically recommend waiting several months after chemotherapy before administering vaccines to allow the immune system to recover sufficiently.
The optimal timing of vaccination should be determined on an individual basis, taking into account the type of chemotherapy received, the patient's overall health, and the specific vaccine being administered.
The Road Ahead: Research and Future Directions
Research is ongoing to better understand the mechanisms of immune recovery after chemotherapy and to develop strategies to accelerate the process. Studies are investigating the use of novel therapies to stimulate bone marrow function and enhance immune reconstitution.
Personalized approaches to chemotherapy are also being explored, with the aim of tailoring treatment regimens to minimize the impact on the immune system while still effectively targeting cancer cells. Advances in immunotherapy are also showing promise in helping to restore immune function after chemotherapy.
Ultimately, a deeper understanding of the complexities of immune recovery will lead to improved outcomes for cancer patients, allowing them to not only survive their disease but also thrive in the years that follow treatment. The path to full immune restoration can be lengthy and filled with challenges, but with vigilant care, proper management, and ongoing research, the future holds promise for quicker and more complete recovery.








:max_bytes(150000):strip_icc()/what-if-you-get-a-cold-during-chemo-5202584_final-b3c1265edc7344fe8ecd26a6f6ae38dd.jpg)