Impaired Skin Integrity Nursing Care Plan

The silent epidemic of impaired skin integrity affects millions worldwide, often stemming from chronic illnesses, age-related vulnerabilities, or inadequate care. Left unaddressed, seemingly minor skin issues can rapidly escalate into severe infections, prolonged hospital stays, and a significant decline in quality of life.
Nurses play a pivotal role in preventing and managing these complications, armed with comprehensive care plans designed to protect and heal compromised skin.
Understanding Impaired Skin Integrity
Impaired skin integrity refers to damage to one or more layers of the skin, disrupting its normal protective functions.
This damage can manifest as pressure ulcers (bedsores), surgical wounds, burns, lacerations, or skin tears, each requiring a tailored approach to care.
The underlying causes are often multifactorial, encompassing pressure, friction, shear, moisture, malnutrition, and underlying medical conditions like diabetes and vascular disease, according to the National Pressure Injury Advisory Panel (NPIAP).
The Nursing Care Plan: A Proactive Approach
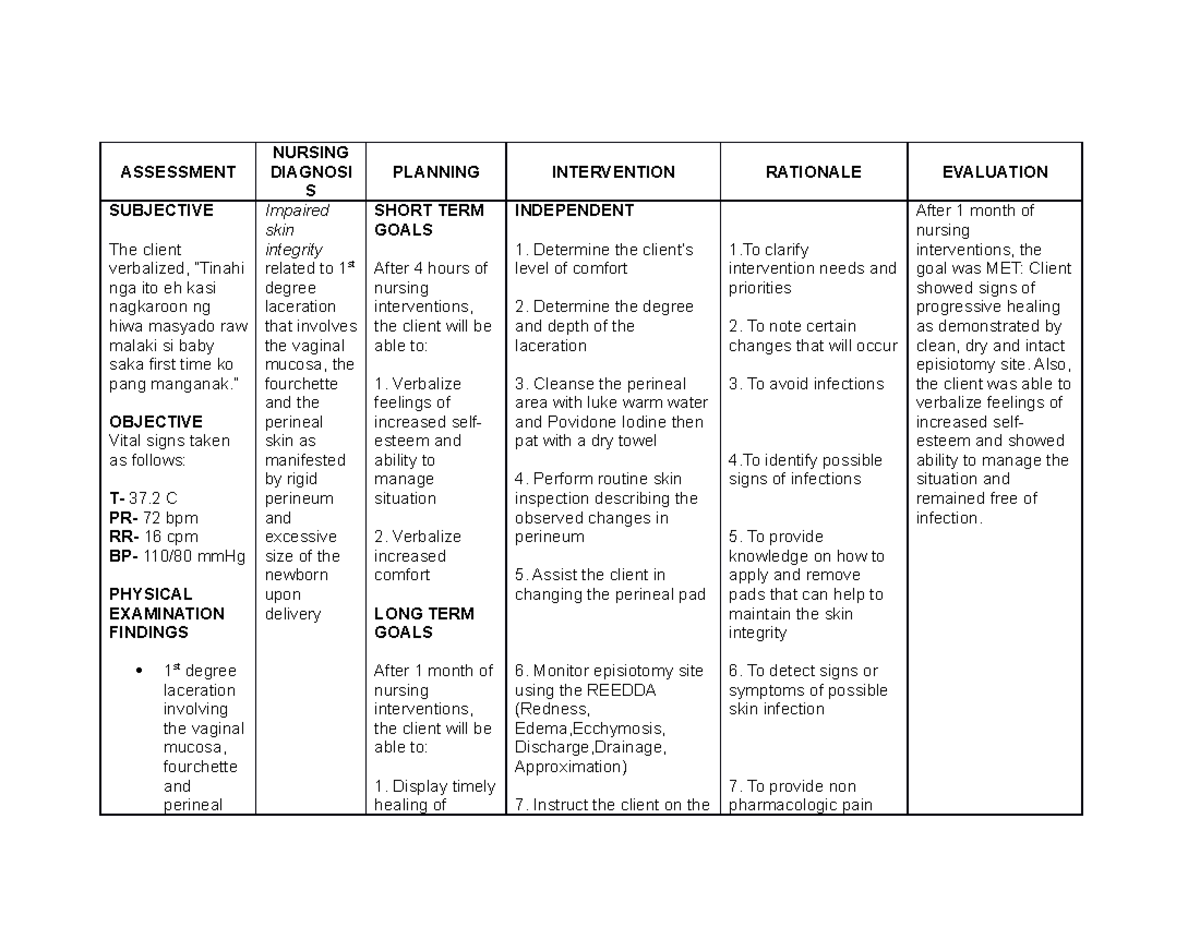
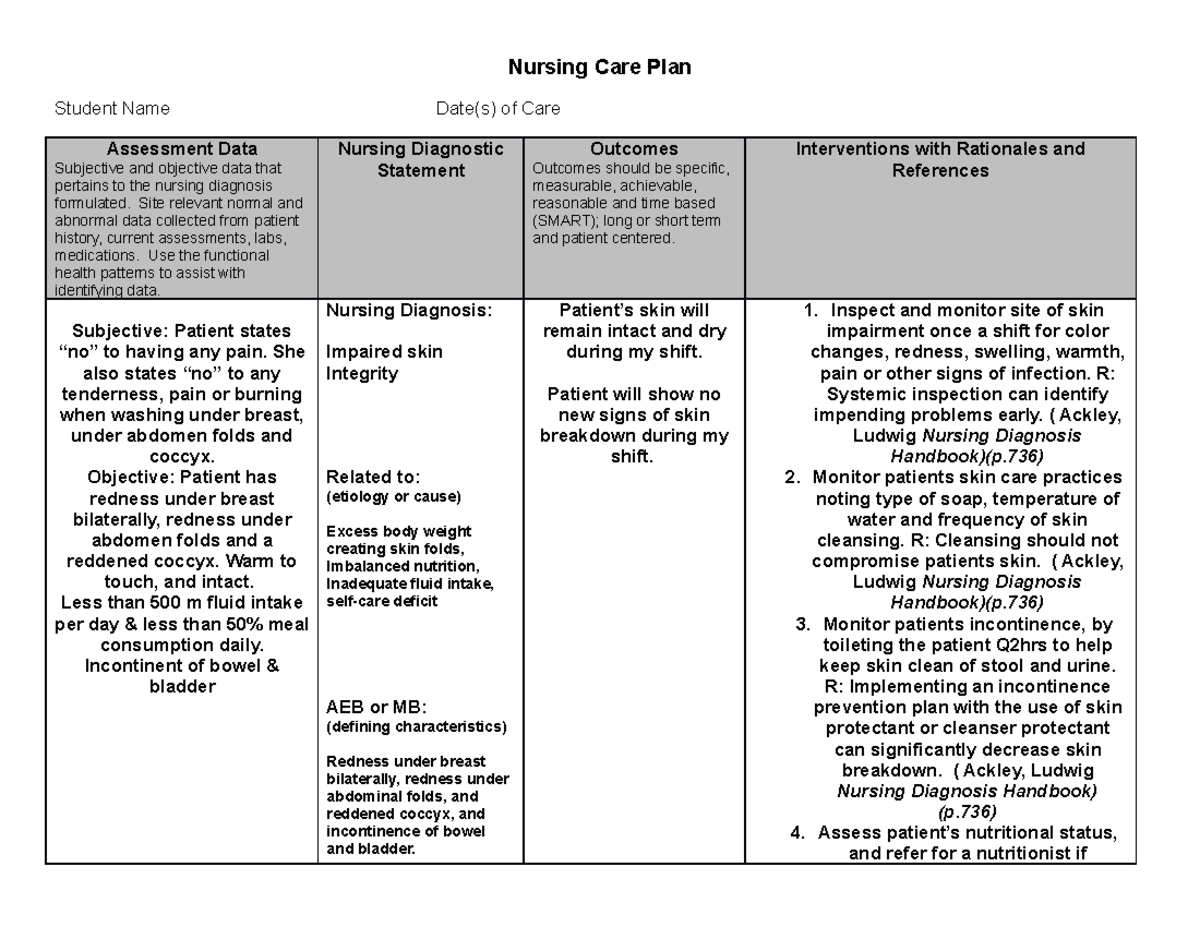
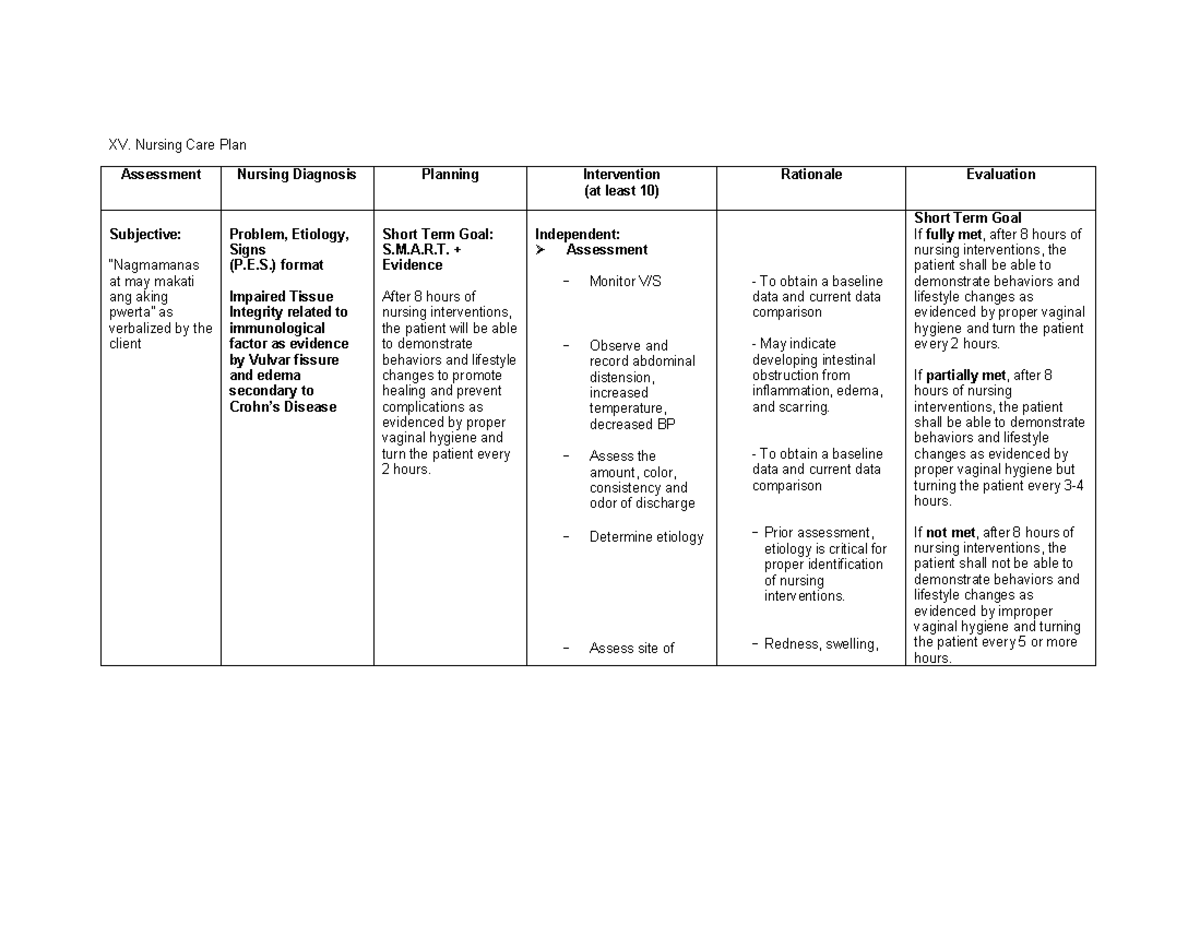
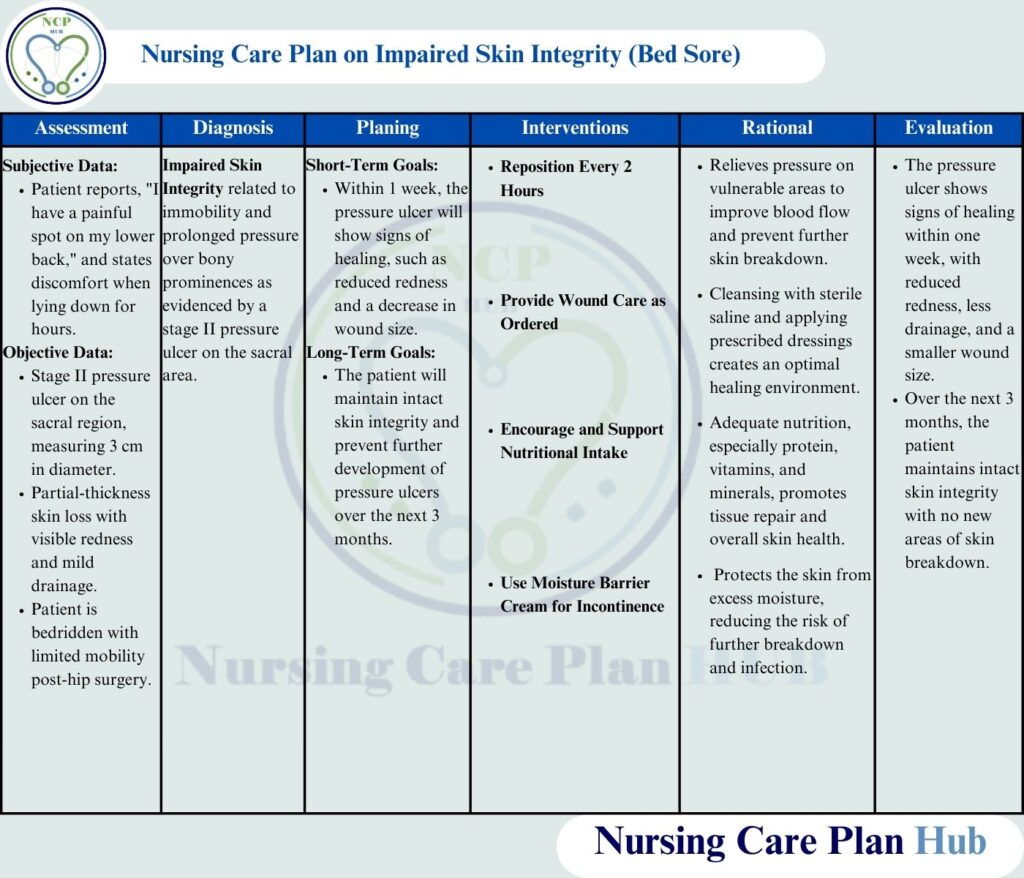
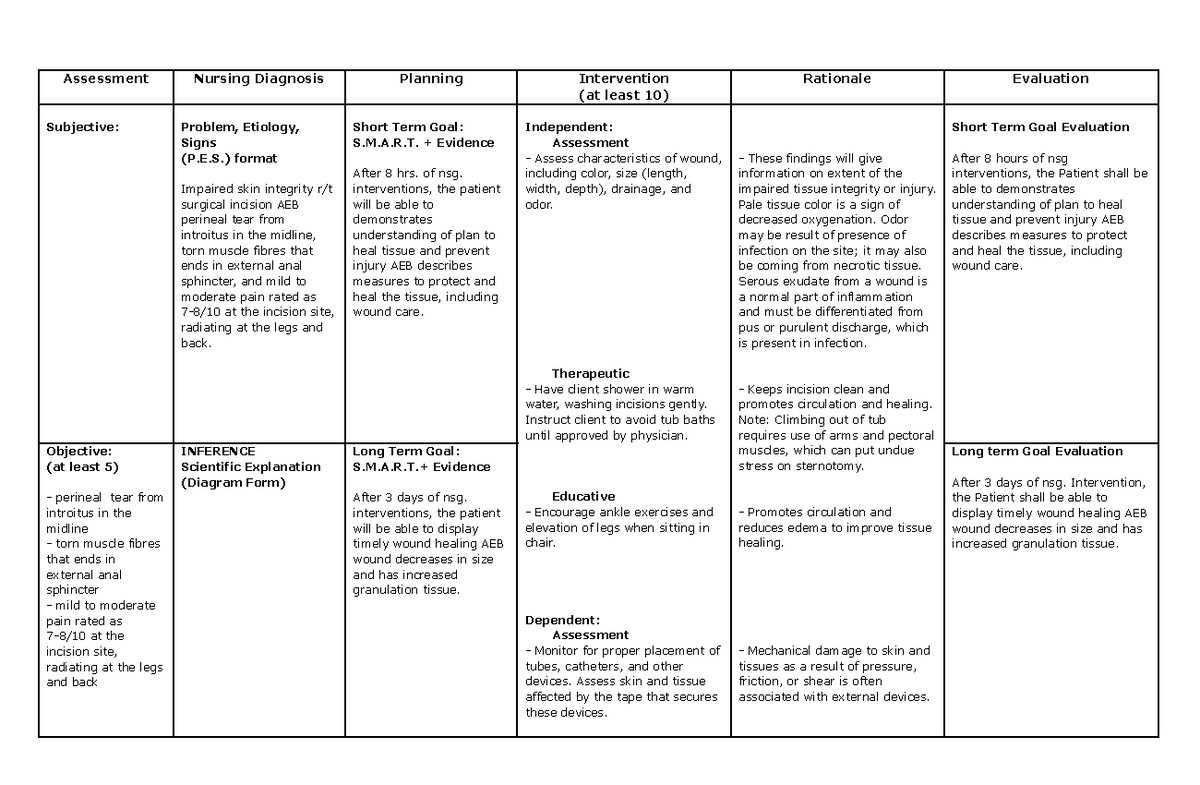
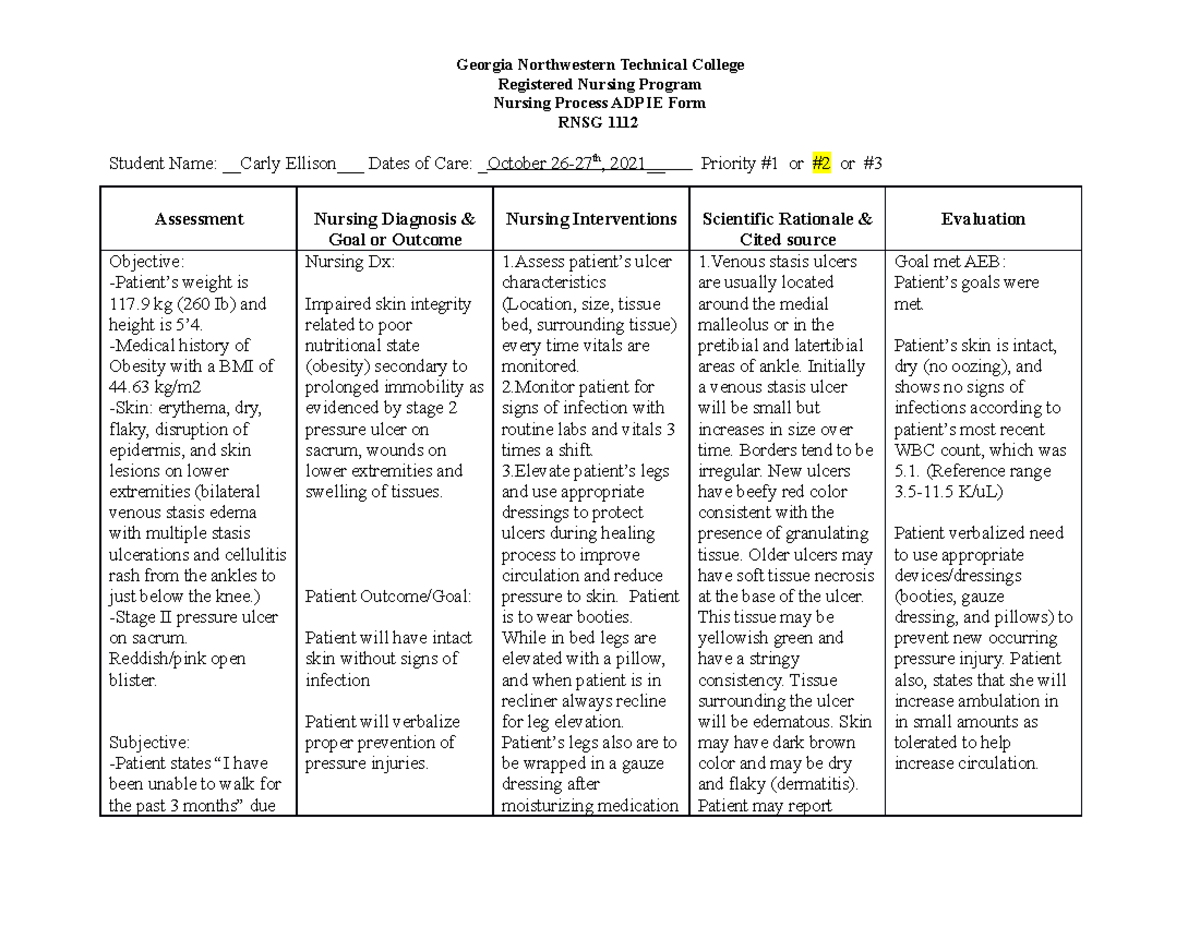
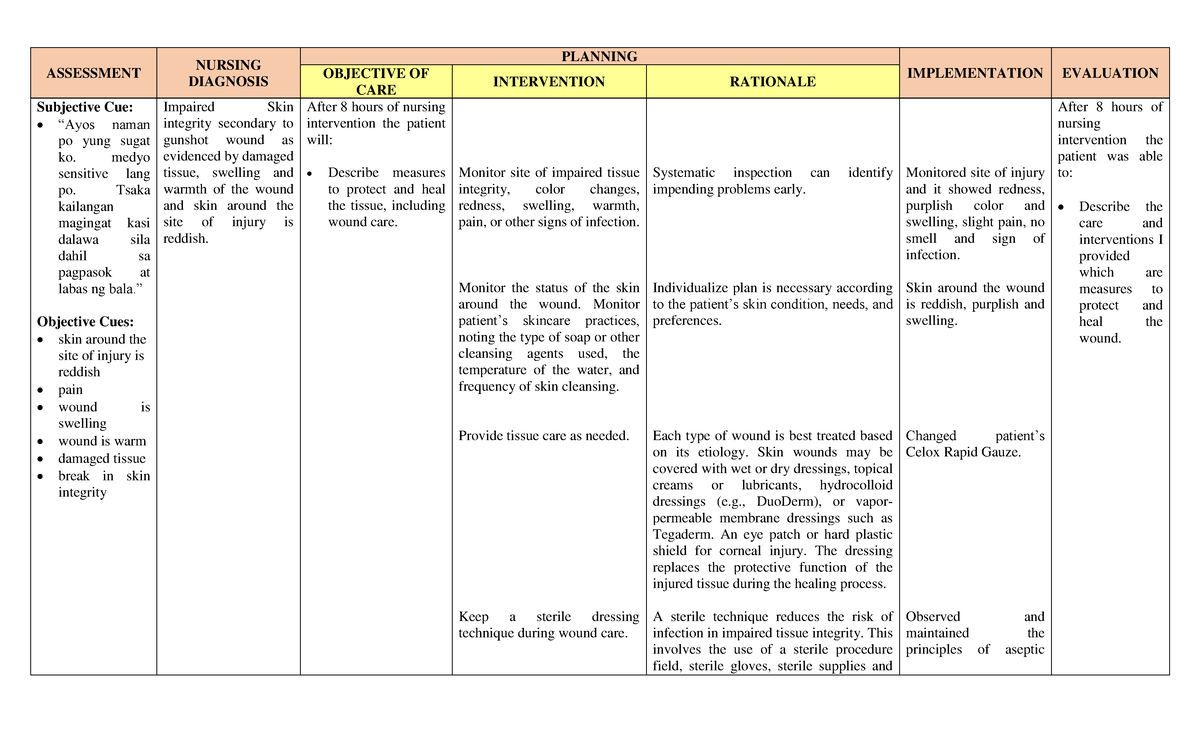
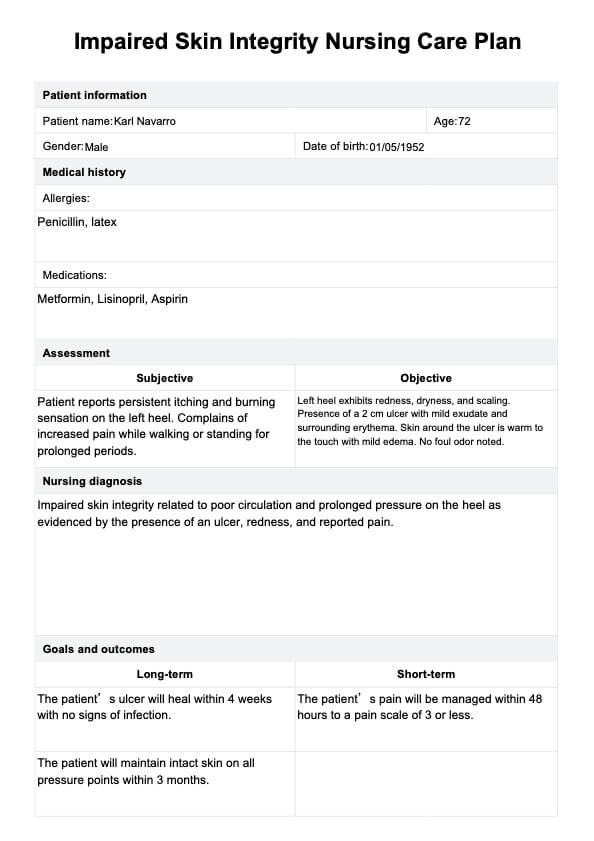
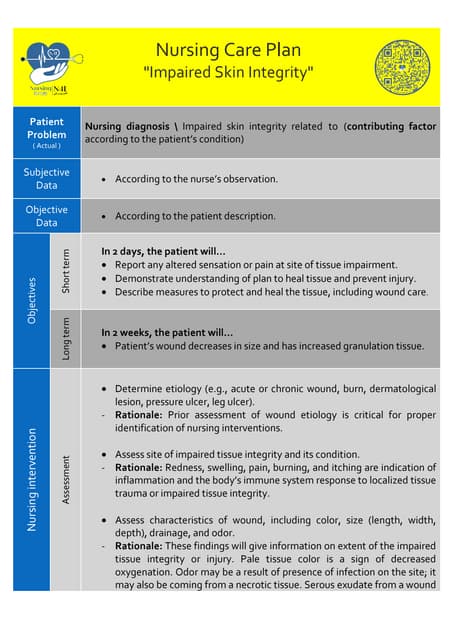
A nursing care plan for impaired skin integrity is a dynamic, individualized document guiding nursing interventions to promote healing and prevent further deterioration.
It begins with a thorough assessment of the patient's skin, risk factors, and overall health status.
This assessment forms the basis for setting specific, measurable, achievable, relevant, and time-bound (SMART) goals, such as "Patient will exhibit no new skin breakdown during hospital stay" or "Wound size will decrease by 1 cm² per week."
Key Components of the Care Plan
The nursing care plan typically encompasses several critical components, each designed to address specific aspects of skin protection and healing.
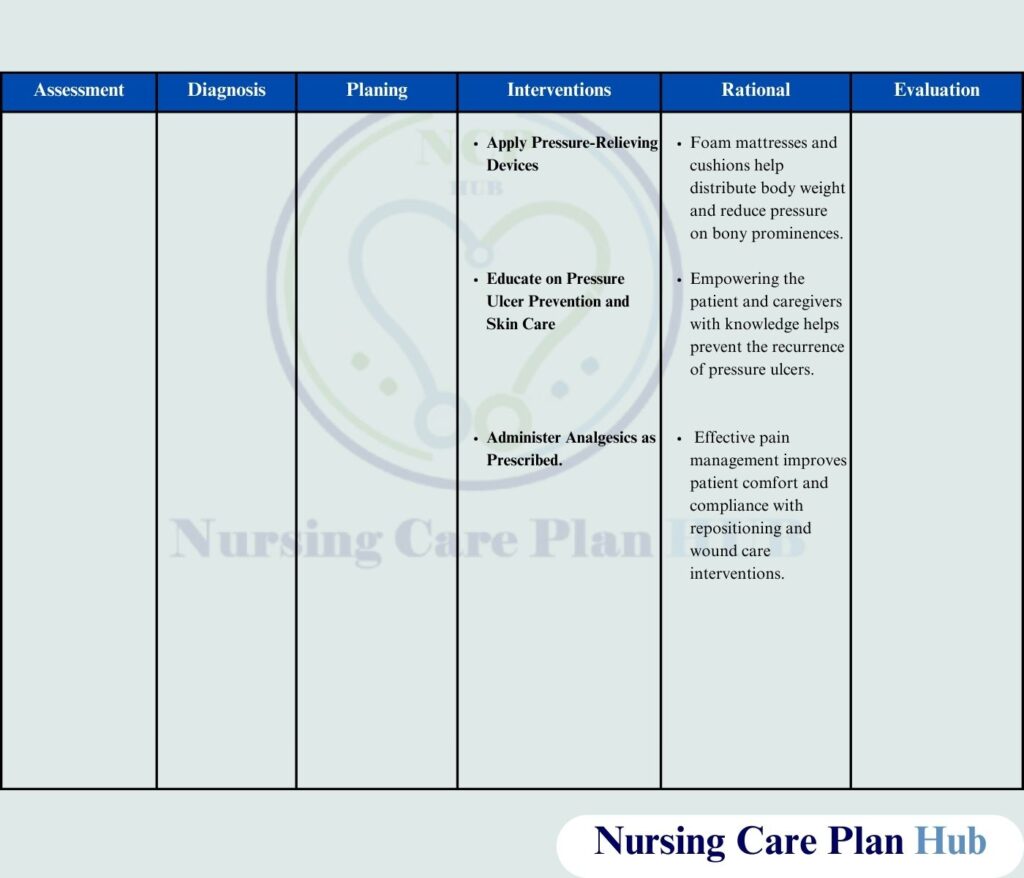
Pressure Relief: This involves regular repositioning (at least every two hours for bedridden patients), the use of pressure-redistributing surfaces like specialized mattresses and cushions, and meticulous attention to bony prominences.
According to the Agency for Healthcare Research and Quality (AHRQ), consistent repositioning is one of the most effective strategies for preventing pressure ulcers.
Skin Hygiene and Moisture Management: Gentle cleansing with pH-balanced cleansers, avoiding harsh soaps, and meticulous drying are crucial.
Moisturizing the skin with appropriate emollients helps maintain skin hydration and elasticity, reducing the risk of tears and breakdown.
Conversely, excessive moisture from incontinence, perspiration, or wound drainage can macerate the skin, increasing vulnerability to damage; barrier creams and absorbent dressings are essential in these situations.
Nutritional Support: Adequate nutrition is vital for wound healing and skin integrity.
A diet rich in protein, vitamins (especially A and C), and minerals (such as zinc) provides the building blocks necessary for tissue repair.
Consultation with a registered dietitian may be necessary to address specific nutritional deficiencies and optimize dietary intake.
Wound Care: Wound care protocols vary depending on the type and severity of the wound.
Debridement (removal of dead or damaged tissue) may be necessary to promote healing; this can be accomplished through various methods, including sharp debridement, enzymatic debridement, and autolytic debridement.
Appropriate wound dressings are selected based on the wound's characteristics (e.g., depth, exudate level, presence of infection) and the goals of treatment; common dressing types include hydrocolloids, hydrogels, alginates, and foams.
Education: Patient and family education is a cornerstone of the care plan.
Patients and their caregivers need to understand the importance of pressure relief, skin hygiene, nutrition, and wound care.
They should be instructed on how to properly reposition the patient, inspect the skin for signs of breakdown, and apply dressings.
Challenges and Emerging Strategies
Despite well-established guidelines, challenges remain in preventing and managing impaired skin integrity.
These challenges include limited resources, staffing shortages, patient non-compliance, and the complexity of managing chronic conditions.
Technology-driven solutions, such as wearable sensors that monitor pressure and moisture levels, are emerging as promising tools for early detection and prevention.
Telehealth and remote monitoring platforms can also facilitate access to expert wound care consultation and support for patients in their homes.
Furthermore, ongoing research is focused on developing novel wound healing therapies, including growth factors, stem cells, and bioengineered skin substitutes.
The Interprofessional Team
Effective management of impaired skin integrity requires a collaborative approach involving nurses, physicians, dietitians, physical therapists, and other healthcare professionals.
Regular interdisciplinary team meetings facilitate communication, coordination of care, and shared decision-making.
This ensures that all aspects of the patient's needs are addressed comprehensively and that the care plan is tailored to their individual circumstances.
A Path Forward
Addressing impaired skin integrity demands a multifaceted approach that combines evidence-based practices, technological advancements, and a commitment to patient-centered care.
By prioritizing prevention, early detection, and individualized treatment plans, healthcare professionals can significantly improve patient outcomes and reduce the burden of this prevalent and often debilitating condition.
Continued education, research, and collaboration are essential to advancing the field and ensuring that all patients receive the best possible care for their skin health.