Meaningful Use Initiatives Include All Of The Following Except
Urgent alert: Confusion and potential compliance failures are spreading throughout the healthcare industry as providers grapple with the complexities of the Meaningful Use program. A significant knowledge gap persists regarding the specific requirements, leading to widespread uncertainty about which elements are, and are not, included within the initiative.
This article clarifies common misconceptions surrounding the Meaningful Use program, addressing prevalent misunderstandings that could jeopardize federal incentive payments and impact patient care.
The Core of Meaningful Use
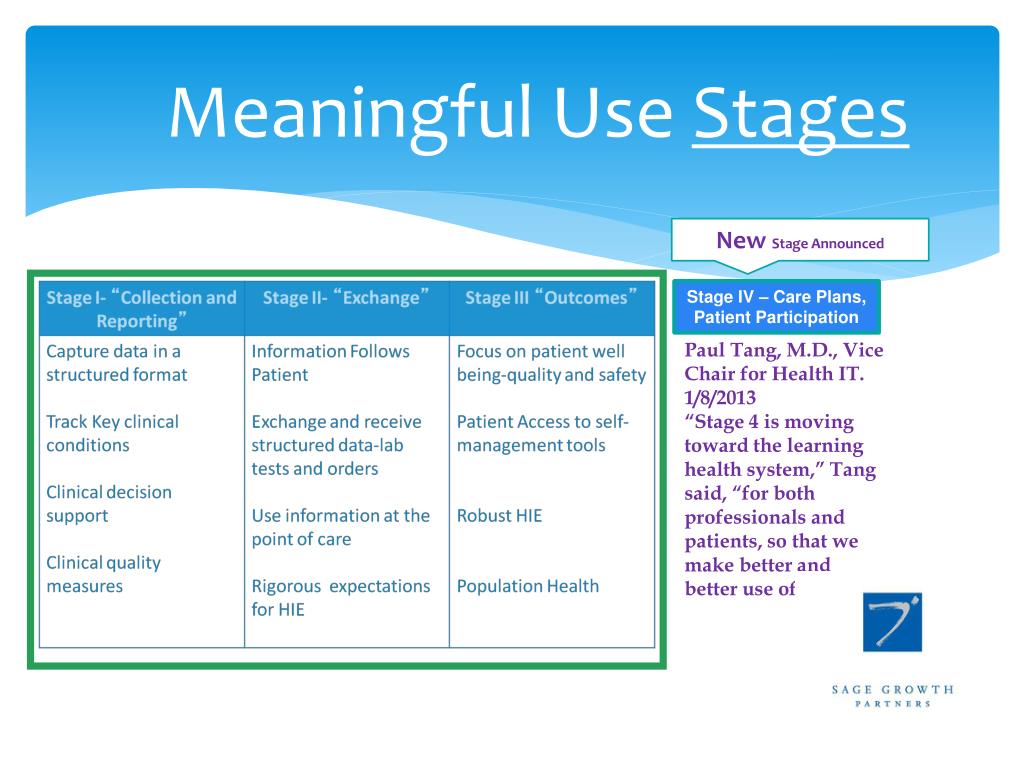
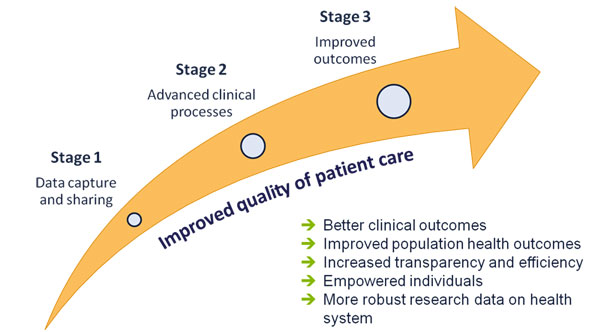
The Meaningful Use program, now transitioned into the Promoting Interoperability (PI) Program under the Medicare Access and CHIP Reauthorization Act (MACRA), aimed to incentivize healthcare providers to adopt and effectively utilize certified Electronic Health Record (EHR) technology.
The goal was to improve patient care coordination, engage patients and families, improve population and public health, and ensure adequate privacy and security protections for personal health information.
Key Components of the Initiative
Several key components defined the requirements for achieving Meaningful Use, varying across stages and program years.
These core objectives included: E-Prescribing, facilitating the electronic transmission of prescriptions to pharmacies; Health Information Exchange, enabling the secure sharing of patient data between providers; and Clinical Decision Support, providing alerts and reminders to clinicians to improve patient safety and quality of care.
Patient engagement was another critical aspect, requiring providers to offer patients access to their health information online through patient portals.
Common Misconceptions: What's NOT Included
Despite these clearly defined objectives, several misconceptions regarding the requirements of Meaningful Use persist within the healthcare community.
One prevailing misconception is that mandatory adoption of a specific EHR vendor was a requirement. The program focused on using certified EHR technology, allowing providers to choose the vendor that best suited their needs.
Another misconception involves guaranteed patient satisfaction scores. While patient engagement was a core objective, Meaningful Use did not mandate specific patient satisfaction targets or link incentive payments directly to patient feedback.
Finally, a common misunderstanding is that complete elimination of paper records was required.
Details about Paper Records
While the program strongly encouraged the transition to electronic records, it did not prohibit the use of paper records altogether.
The emphasis was on utilizing certified EHR technology for core functions and promoting interoperability, not mandating a paperless environment.
This flexibility was crucial for accommodating practices with unique needs and for managing workflows during the transition period.
Consequences of Misunderstanding
Misinterpreting the requirements of Meaningful Use, or the subsequent Promoting Interoperability Program, can lead to significant consequences for healthcare providers.
Failure to meet the program's objectives can result in reduced Medicare reimbursement rates, impacting financial stability.
Furthermore, misunderstanding the program can hinder efforts to improve patient care and achieve true interoperability, ultimately affecting the quality of healthcare delivery.
Expert Perspectives
Dr. Emily Carter, a leading expert in health informatics, emphasizes the importance of continuous education.
"Healthcare providers must stay informed about the evolving requirements of the Promoting Interoperability Program to avoid compliance issues and maximize the benefits of EHR technology," she warns.
"Regular training and access to reliable resources are essential for navigating the complexities of this initiative."
Moving Forward
The transition from Meaningful Use to the Promoting Interoperability Program represents a continued commitment to leveraging technology to improve healthcare.
Providers must actively seek clarification on any uncertainties regarding the program's requirements and ensure they are utilizing certified EHR technology effectively.
Ongoing monitoring of program updates and engagement with industry experts are crucial for success and for delivering high-quality, patient-centered care.
The Centers for Medicare & Medicaid Services (CMS) offers resources and support for providers participating in the Promoting Interoperability Program, including educational materials and technical assistance.
Providers are encouraged to utilize these resources to address any questions or concerns and ensure compliance with program requirements.

![Meaningful Use Initiatives Include All Of The Following Except What Are Strategic Initiatives? [+ Examples] | HR Glossary – AIHR](https://www.aihr.com/wp-content/uploads/How-To-Develop-Strategic-Initiatives1.png)







![Meaningful Use Initiatives Include All Of The Following Except [ANSWERED] Common ethical dilemmas include all of the following except](https://media.kunduz.com/media/sug-question-candidate/20231029042951843354-6145030.jpg?h=512)




