Oral Antibiotics For Gram Negative Bacteria
The increasing prevalence of antibiotic-resistant Gram-negative bacteria poses a significant threat to global public health, prompting renewed focus on developing and utilizing effective treatment strategies. While intravenous antibiotics have traditionally been the mainstay for serious Gram-negative infections, recent research and clinical experience are highlighting the potential of oral antibiotics in select cases, offering convenience and reducing healthcare costs.
This shift towards oral options represents a paradigm change in treating these infections. It has implications for both patients and healthcare systems. This article explores the evolving landscape of oral antibiotics for Gram-negative bacteria, examining their efficacy, limitations, and the factors influencing their appropriate use.
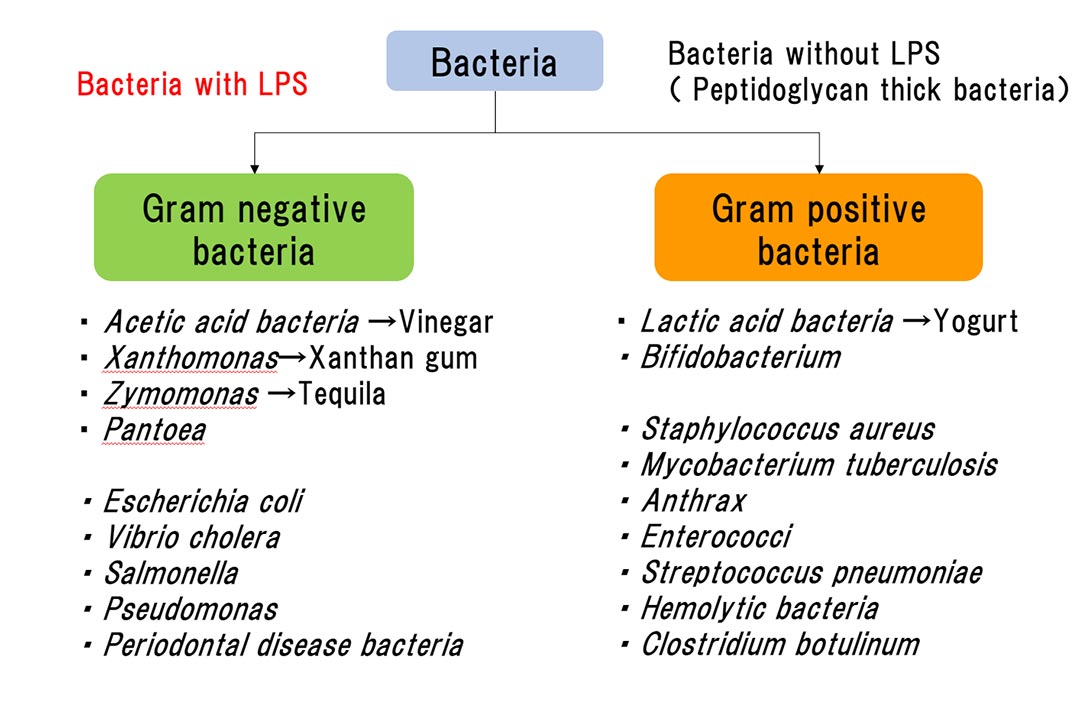
Understanding Gram-Negative Bacteria and Antibiotic Resistance
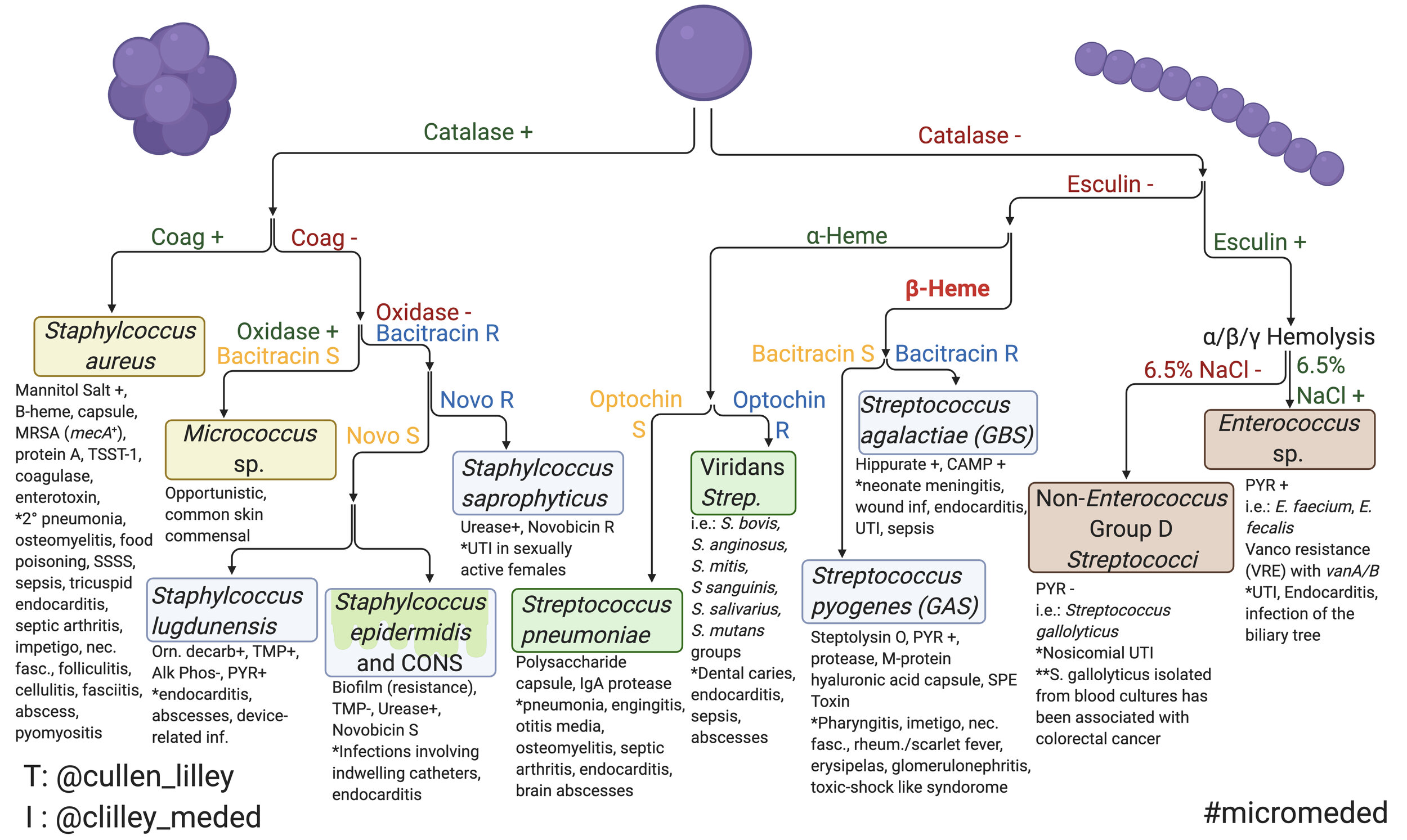
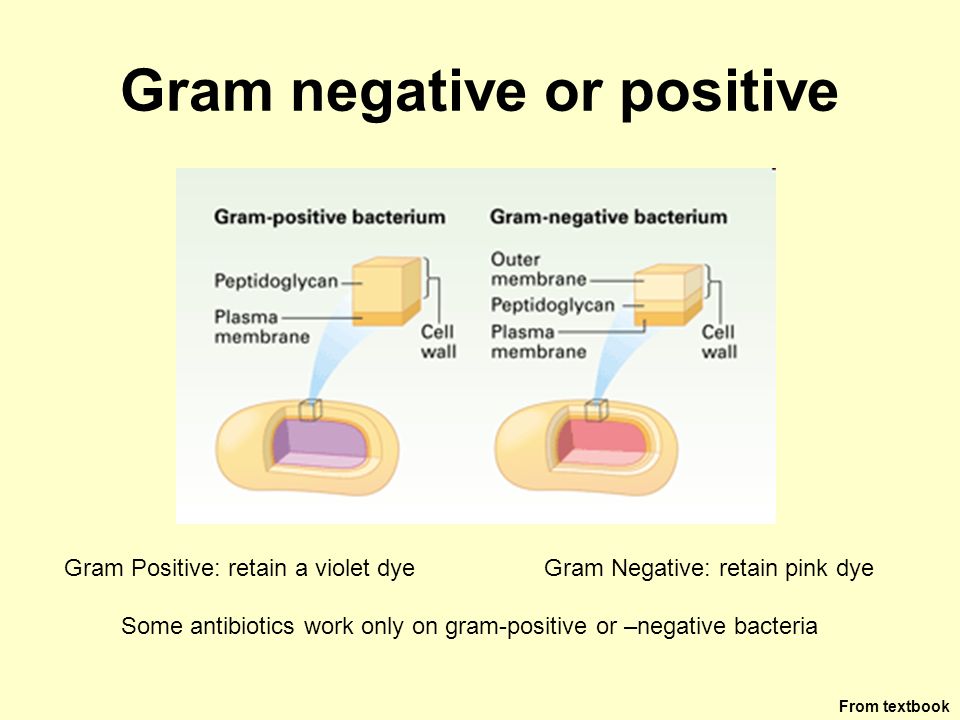
Gram-negative bacteria are a diverse group of microorganisms characterized by their complex cell wall structure, which makes them inherently more resistant to certain antibiotics compared to Gram-positive bacteria. Infections caused by Gram-negative bacteria, such as Escherichia coli (E. coli), Klebsiella pneumoniae, and Pseudomonas aeruginosa, can range from urinary tract infections (UTIs) to pneumonia and bloodstream infections.
The rise of antibiotic resistance among Gram-negative bacteria is a global concern fueled by factors such as overuse of antibiotics, inadequate infection control practices, and the bacteria's ability to acquire resistance genes. The World Health Organization (WHO) has identified several antibiotic-resistant Gram-negative bacteria as critical threats to human health.
The Role of Oral Antibiotics
Historically, severe Gram-negative infections have been primarily treated with intravenous antibiotics administered in hospital settings. However, the development of new oral antibiotics and improved understanding of pharmacokinetics and pharmacodynamics have expanded the potential for outpatient treatment.
Oral antibiotics offer several advantages. These include reducing the need for hospitalization, lowering healthcare costs, and improving patient convenience and quality of life.
Key Oral Antibiotics for Gram-Negative Infections
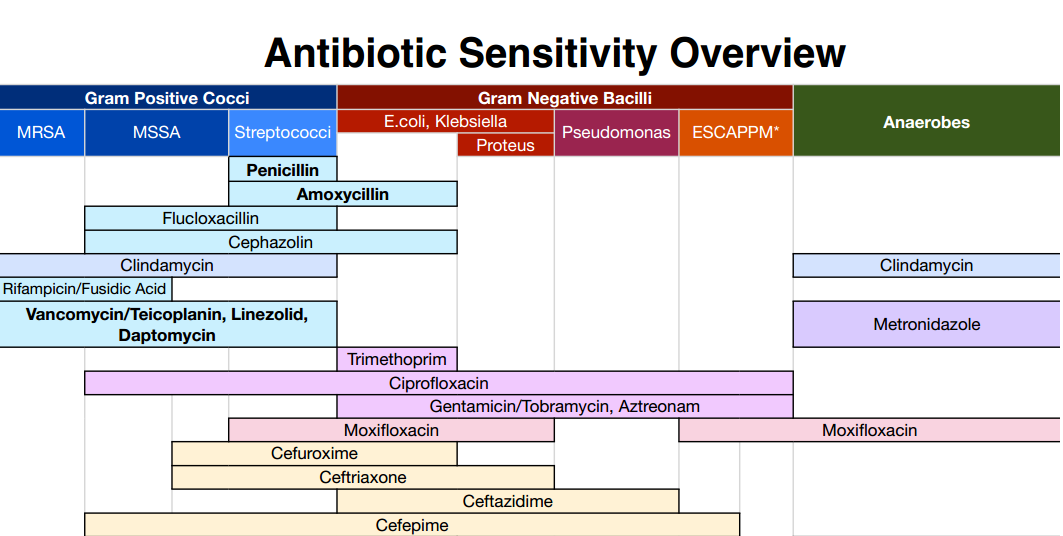
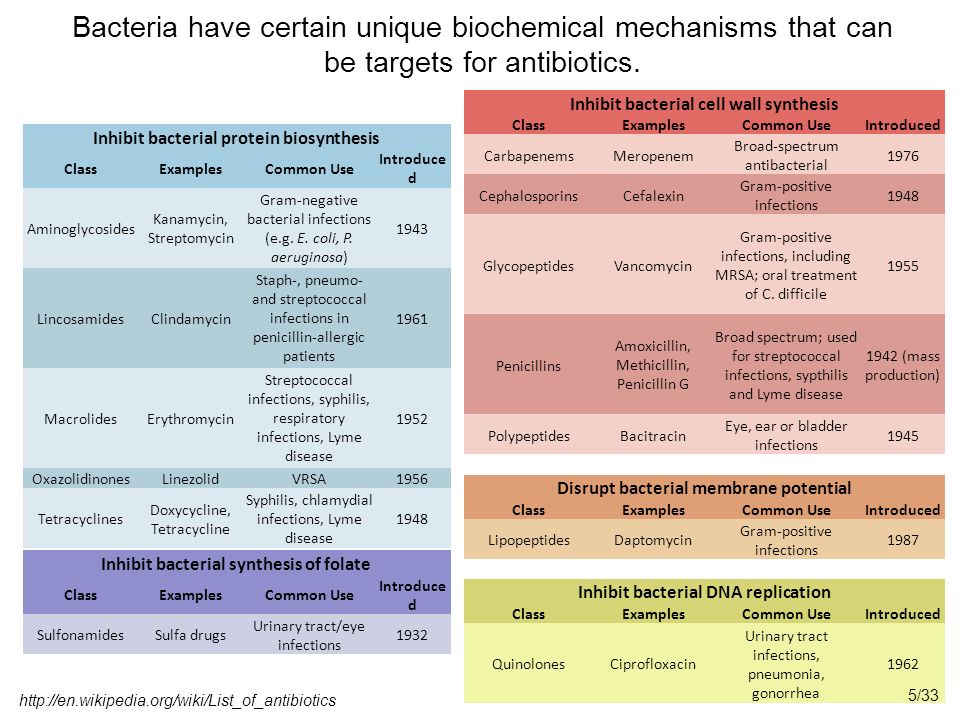
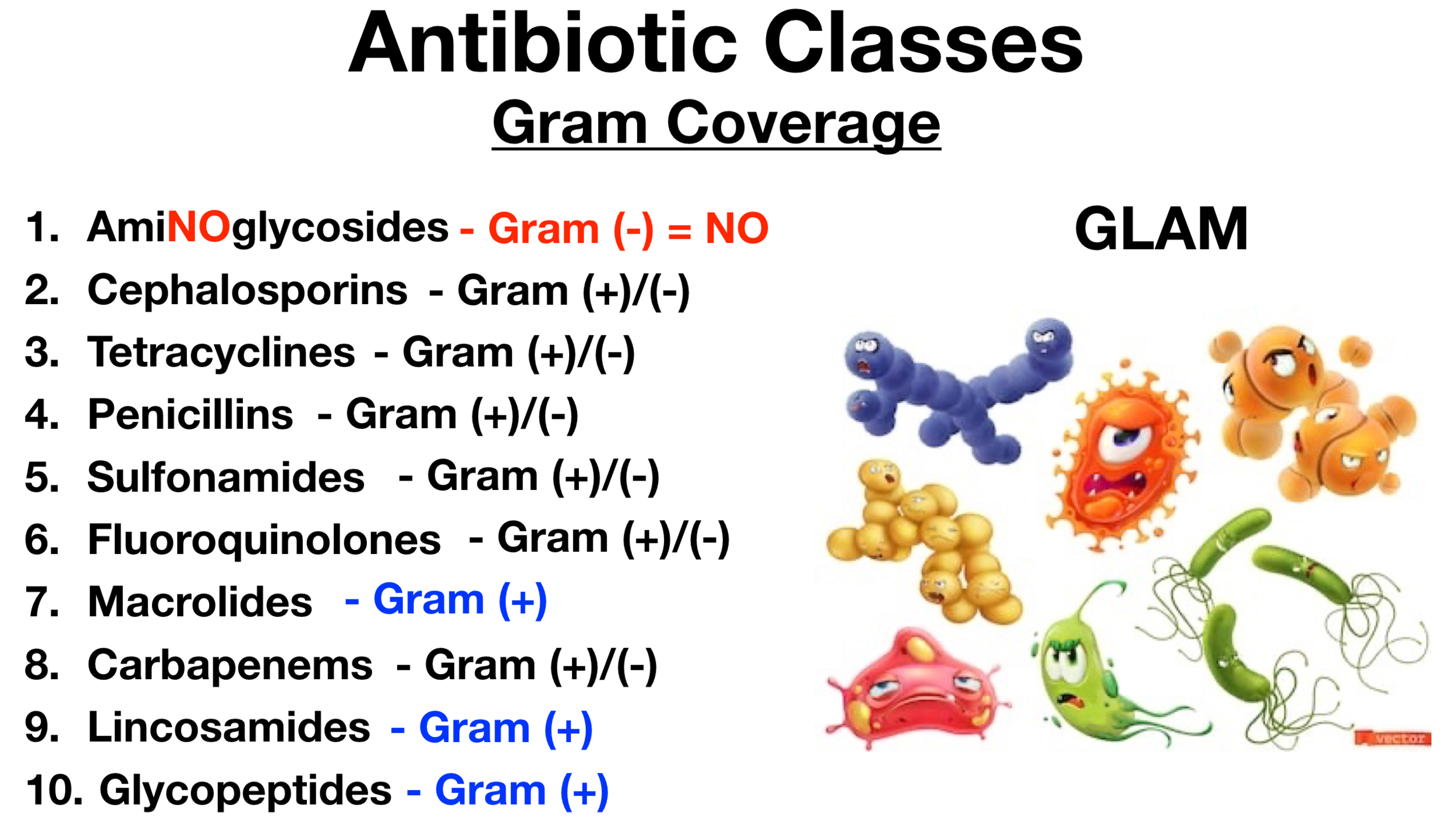
Several oral antibiotics have demonstrated efficacy against specific Gram-negative bacteria in certain clinical scenarios. These include fluoroquinolones (e.g., ciprofloxacin, levofloxacin), trimethoprim-sulfamethoxazole (TMP-SMX), and nitrofurantoin. More recently, newer agents like cefiderocol (administered intravenously but highlighting a commitment to novel solutions) and oral formulations of older drugs are being explored.
Fluoroquinolones have been widely used to treat UTIs, respiratory tract infections, and some skin and soft tissue infections. However, their use has been tempered by concerns about increasing resistance and potential adverse effects, including tendon rupture and C. difficile infection.
TMP-SMX remains a valuable option for uncomplicated UTIs. Resistance patterns vary geographically, so local susceptibility data should always guide treatment decisions.
Nitrofurantoin is primarily used for UTIs and is generally well-tolerated, with a low propensity for developing resistance. It is often preferred for uncomplicated UTIs, especially in areas with high fluoroquinolone resistance.
Considerations for Oral Antibiotic Use
Selecting the appropriate oral antibiotic for a Gram-negative infection requires careful consideration of several factors. These include the severity of the infection, the patient's medical history, local resistance patterns, and the antibiotic's pharmacokinetic and pharmacodynamic properties.
It is essential to obtain appropriate cultures and susceptibility testing to identify the causative organism and determine its susceptibility to various antibiotics. This information guides the selection of the most effective antibiotic and helps to minimize the development of resistance.
Patient adherence is crucial for successful oral antibiotic therapy. Healthcare providers should educate patients about the importance of taking the medication as prescribed and completing the full course of treatment, even if they start feeling better.
Challenges and Future Directions
Despite the potential benefits of oral antibiotics, several challenges remain in their widespread adoption for Gram-negative infections. One major challenge is the increasing prevalence of antibiotic resistance. Continued surveillance of resistance patterns is crucial to inform treatment guidelines and identify emerging threats.
The development of new oral antibiotics with novel mechanisms of action is essential to combat resistance. Research efforts are focused on identifying new drug targets and developing agents that can overcome existing resistance mechanisms.
Antimicrobial stewardship programs play a vital role in promoting the appropriate use of antibiotics and minimizing the development of resistance. These programs implement strategies to optimize antibiotic selection, dosing, and duration of therapy, ensuring that antibiotics are used only when necessary and for the shortest effective duration.
One example of the impact of antibiotic resistance is the personal story of Maria Rodriguez, a 68-year-old woman who suffered a complicated UTI caused by a multi-drug resistant strain of E. coli. Initially treated with multiple courses of intravenous antibiotics, she eventually responded to a specific oral antibiotic after susceptibility testing revealed its efficacy.
Maria's experience underscores the importance of personalized medicine and tailoring antibiotic therapy to the specific needs of each patient. It highlights the growing urgency to find alternatives to current treatment options.
Conclusion
Oral antibiotics are increasingly recognized as a valuable tool in the management of Gram-negative infections. The correct application of these drugs offers potential benefits in terms of cost, patient compliance, and accessibility of treatment.
However, the use of oral antibiotics must be guided by careful consideration of several factors, including the severity of the infection, local resistance patterns, and patient-specific characteristics. Continued research and development of new antibiotics, along with robust antimicrobial stewardship programs, are essential to ensure the continued effectiveness of oral antibiotics in the fight against antibiotic-resistant Gram-negative bacteria.