The Sciatic Nerve Is A Combination Of Which Two Nerves
For individuals experiencing the searing pain of sciatica, understanding the underlying anatomy can be crucial in managing and potentially preventing future episodes. While commonly referred to as a single nerve, the sciatic nerve is actually a confluence of two distinct nerves originating in the lower spine. This intricate anatomical detail plays a pivotal role in how sciatica presents and how it's treated.
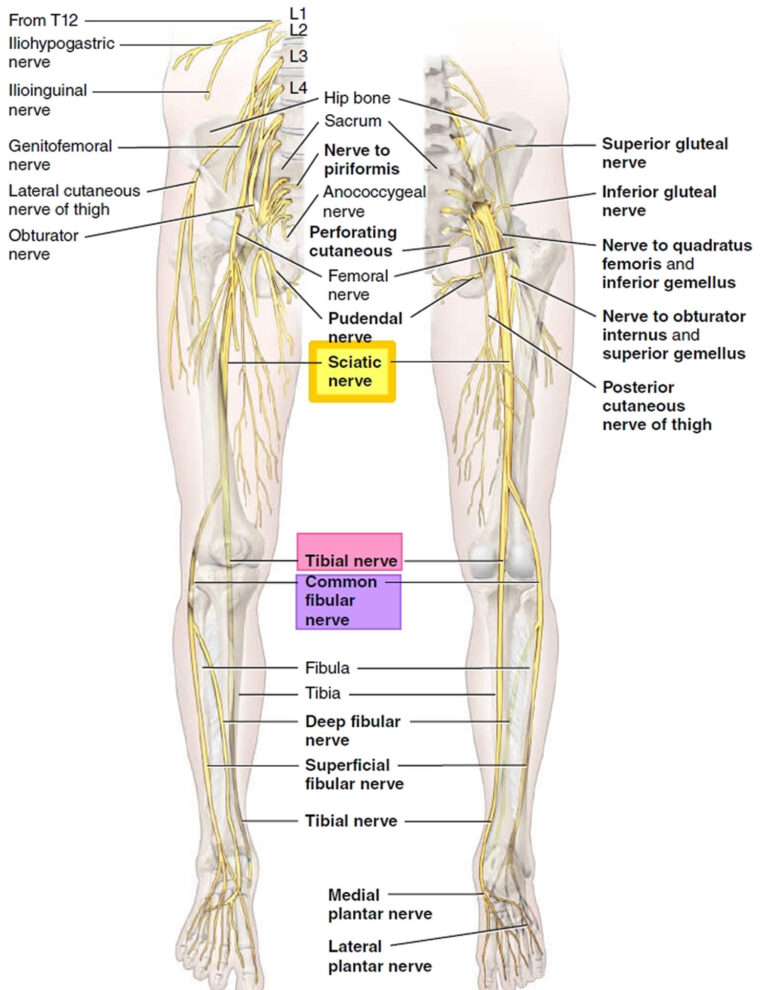
Understanding that the sciatic nerve is a combination of two distinct nerves—the tibial nerve and the common fibular (peroneal) nerve—is essential for both medical professionals and patients alike. This knowledge impacts diagnostic approaches, treatment strategies, and patient education. Ignoring this anatomical reality could lead to ineffective or misdirected interventions.
The Sciatic Nerve: A Union of Two
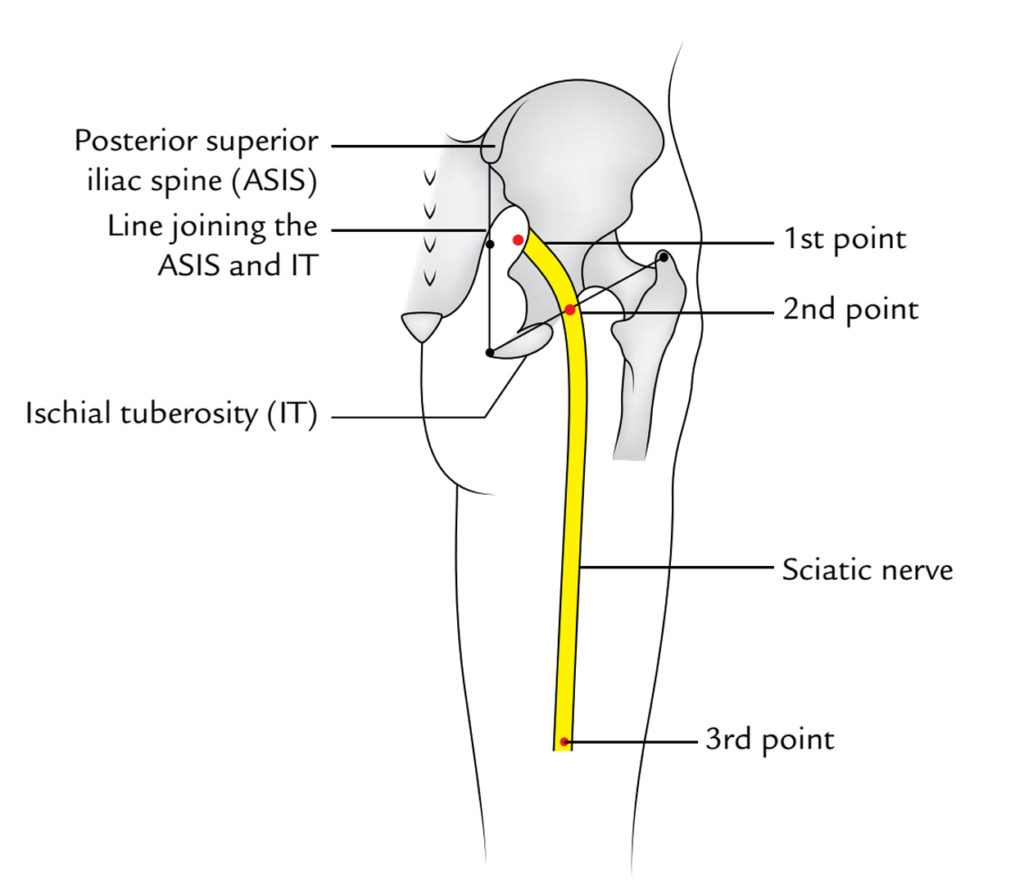
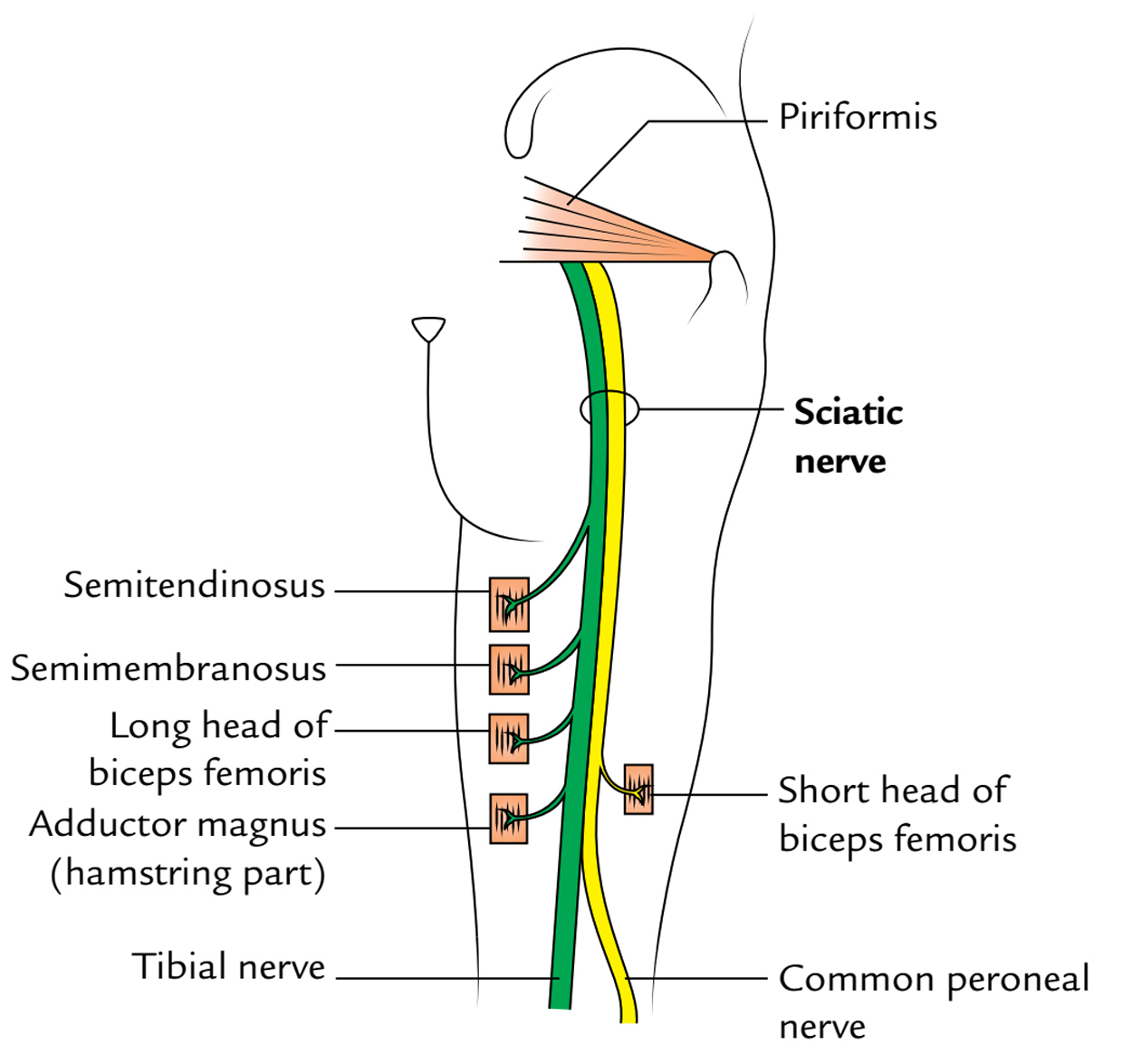
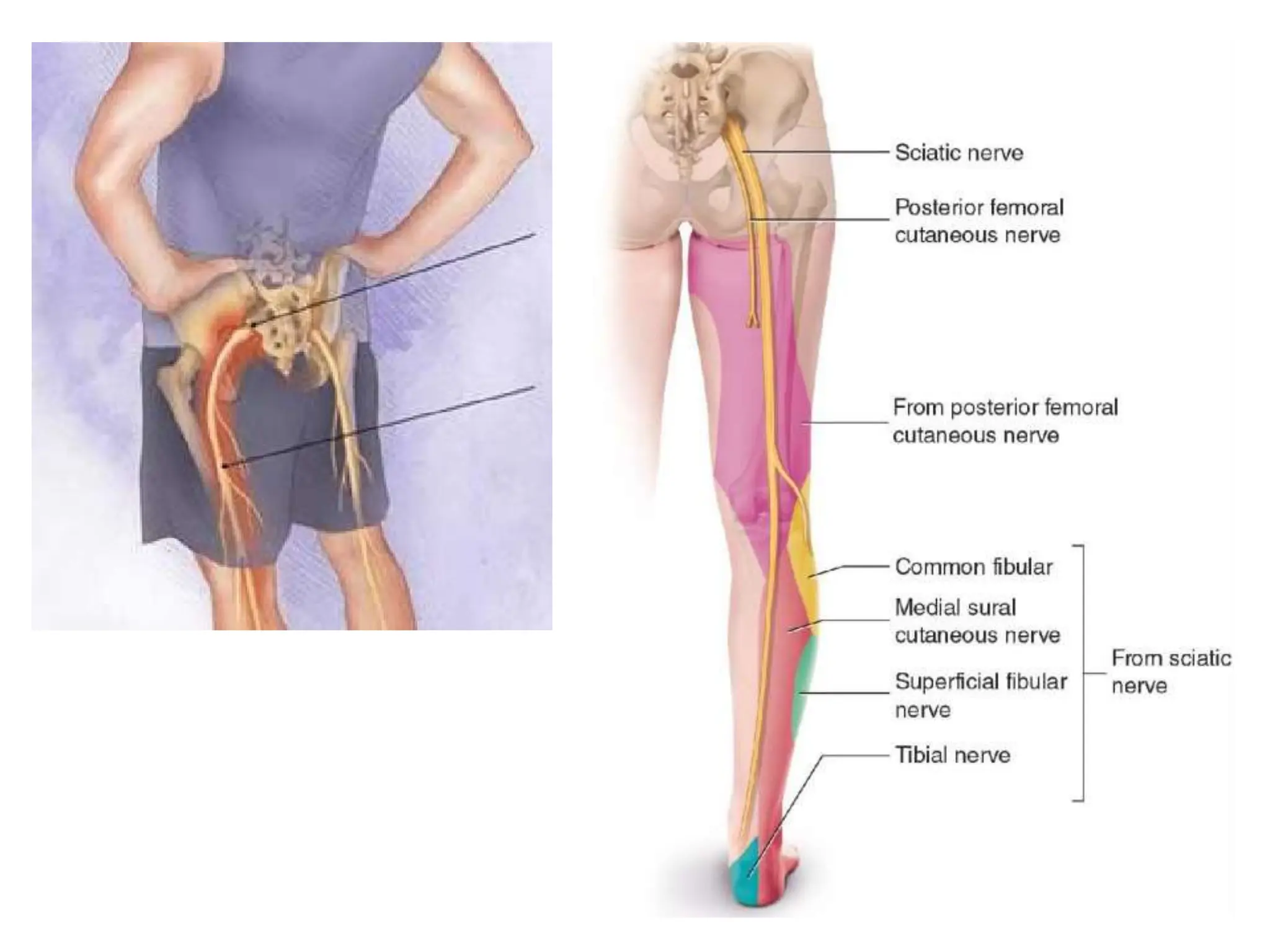
The sciatic nerve, the largest and longest nerve in the human body, originates in the lumbar spine, specifically from nerve roots L4 through S3. These nerve roots converge to form two distinct nerves that travel together for a portion of their journey down the leg.
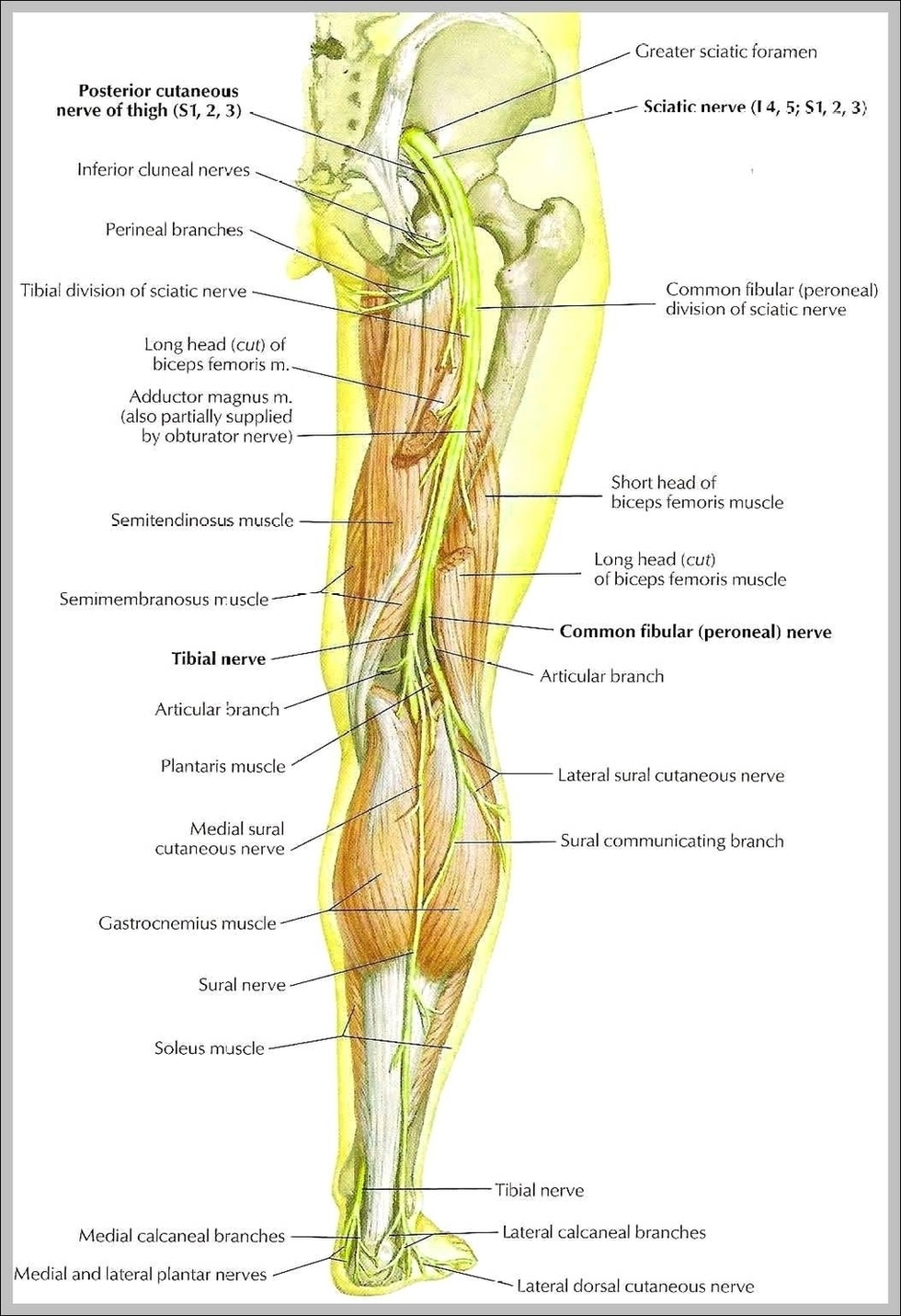
The tibial nerve is one of the two primary components. It is responsible for the innervation of the posterior compartment of the thigh, leg, and the plantar (sole) surface of the foot.
This nerve controls muscles involved in knee flexion, ankle plantarflexion (pointing the toes), and toe flexion. It also provides sensory information from the sole of the foot.
The second major component is the common fibular (peroneal) nerve. This nerve innervates the anterior and lateral compartments of the leg and the dorsum (top) of the foot.
It controls muscles involved in ankle dorsiflexion (lifting the foot), ankle eversion (turning the sole outward), and toe extension. Sensation from the top of the foot and the lateral aspect of the lower leg is also transmitted via this nerve.
Why This Matters: Clinical Implications
The fact that the sciatic nerve comprises two distinct nerves has significant clinical implications. Understanding this anatomy helps explain the varying symptoms patients experience with sciatica.
For instance, damage primarily affecting the tibial nerve component might present with difficulty plantarflexing the foot or sensory loss on the sole. Conversely, damage mainly affecting the common fibular nerve may result in foot drop, where the individual struggles to lift the foot, and sensory changes on the top of the foot.
Diagnostic Precision
Knowing the separate functions of the tibial and common fibular nerves allows for more precise diagnoses. Physicians can use specific neurological examinations to determine which component of the sciatic nerve is primarily affected.
Electromyography (EMG) and nerve conduction studies can further pinpoint the location and severity of nerve damage. This information is critical in guiding treatment decisions.
Tailored Treatment Strategies
Treatment approaches can be tailored based on which nerve is predominantly involved. For example, physical therapy exercises can be designed to specifically target muscles innervated by the tibial or common fibular nerve.
In cases of nerve compression, surgical decompression might focus on relieving pressure on the specific nerve component that is affected. This targeted approach can improve outcomes and minimize unnecessary interventions.
A Patient's Perspective: Understanding the Pain
For those suffering from sciatica, knowing the underlying anatomy can empower them to better understand their condition. Learning about the distinct functions of the tibial and common fibular nerves can help patients recognize specific symptoms and communicate them more effectively to their healthcare providers.
This understanding can also facilitate greater engagement in their own treatment plan, whether it involves physical therapy, medication, or other interventions. Active participation and a clear understanding of the condition is often linked to better recovery.
"When my doctor explained that the sciatic nerve was actually two nerves working together, it made so much more sense," shares Sarah Miller, a sciatica patient. "Knowing that foot drop was related to the common fibular nerve helped me understand why I was struggling to walk normally and motivated me to diligently follow my physical therapy exercises."
Looking Ahead: Advancing Sciatica Treatment
Ongoing research continues to explore the complexities of the sciatic nerve and its individual components. By further refining our understanding of the tibial and common fibular nerves, medical professionals can develop even more effective and targeted treatment strategies for sciatica.
Future advancements may include more precise diagnostic imaging techniques and innovative therapeutic interventions. These developments hold the promise of alleviating the debilitating pain associated with sciatica and improving the quality of life for millions of sufferers.
Ultimately, recognizing that the sciatic nerve is not a single entity but rather a carefully orchestrated union of the tibial and common fibular nerves is a fundamental step toward more effective diagnosis, treatment, and management of this common and often debilitating condition. Increased awareness of this anatomical reality can empower both clinicians and patients to navigate the complexities of sciatica and strive for optimal outcomes.