Top 10 Denials In Medical Billing
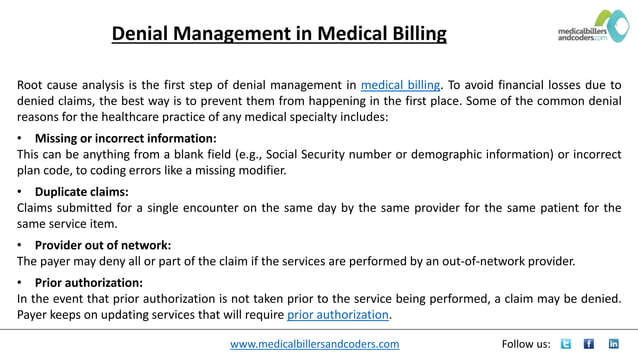
Navigating the complex world of medical billing can be a daunting task for healthcare providers. A significant hurdle they face is claim denials, which not only disrupt cash flow but also add administrative burden. Understanding the leading reasons for these denials is crucial for improving billing practices and ensuring timely reimbursement.
The healthcare industry loses significant revenue due to denied claims. This article delves into the top 10 reasons for medical billing denials, providing insights into why they occur and how healthcare providers can mitigate them.
Top 10 Medical Billing Denials
1. Duplicate Claims
Submitting the same claim more than once is a common error leading to denial. This often happens when a claim is resubmitted without properly checking its prior status, or due to system errors within the billing software.
2. Lack of Medical Necessity
Services deemed not medically necessary by the payer are frequently denied. This means the documentation doesn't adequately justify the treatment or procedure based on the patient's diagnosis and condition.
3. Prior Authorization Issues
Many insurance plans require prior authorization for certain procedures and medications. Failure to obtain this authorization before the service is rendered almost always results in denial.
4. Incorrect Coding
Using incorrect or outdated ICD-10, CPT, or HCPCS codes is a major contributor to claim denials. Accurate coding is paramount for proper reimbursement.
5. Coverage Terminated
A claim will be denied if the patient's insurance coverage was not active on the date of service. This could be due to a lapse in payment, a change in insurance plans, or other administrative issues.
6. Non-Covered Services
Some insurance plans simply do not cover certain services or procedures. It's essential to verify coverage before providing care to avoid unexpected denials.
7. Timely Filing Limit Exceeded
Every insurance payer has a timely filing deadline, which is the period within which a claim must be submitted after the date of service. Submitting a claim after this deadline will result in denial.
8. Patient Ineligible
A claim may be denied if the patient listed on the claim does not match the insurance policyholder's records. This can arise from typographical errors, incorrect policy information, or patients using the incorrect insurance.
9. Missing Information
Incomplete claims, lacking essential details like the patient's name, date of birth, policy number, or provider information, are routinely rejected. Thoroughness is key when preparing claims.
10. Coordination of Benefits (COB) Issues
When a patient has multiple insurance policies, it is essential to correctly determine the primary and secondary payers. Errors in COB can lead to claims being denied or delayed.
Impact and Mitigation Strategies
Claim denials have a cascading effect. They reduce revenue, increase administrative costs, and potentially harm patient satisfaction if billing disputes arise.
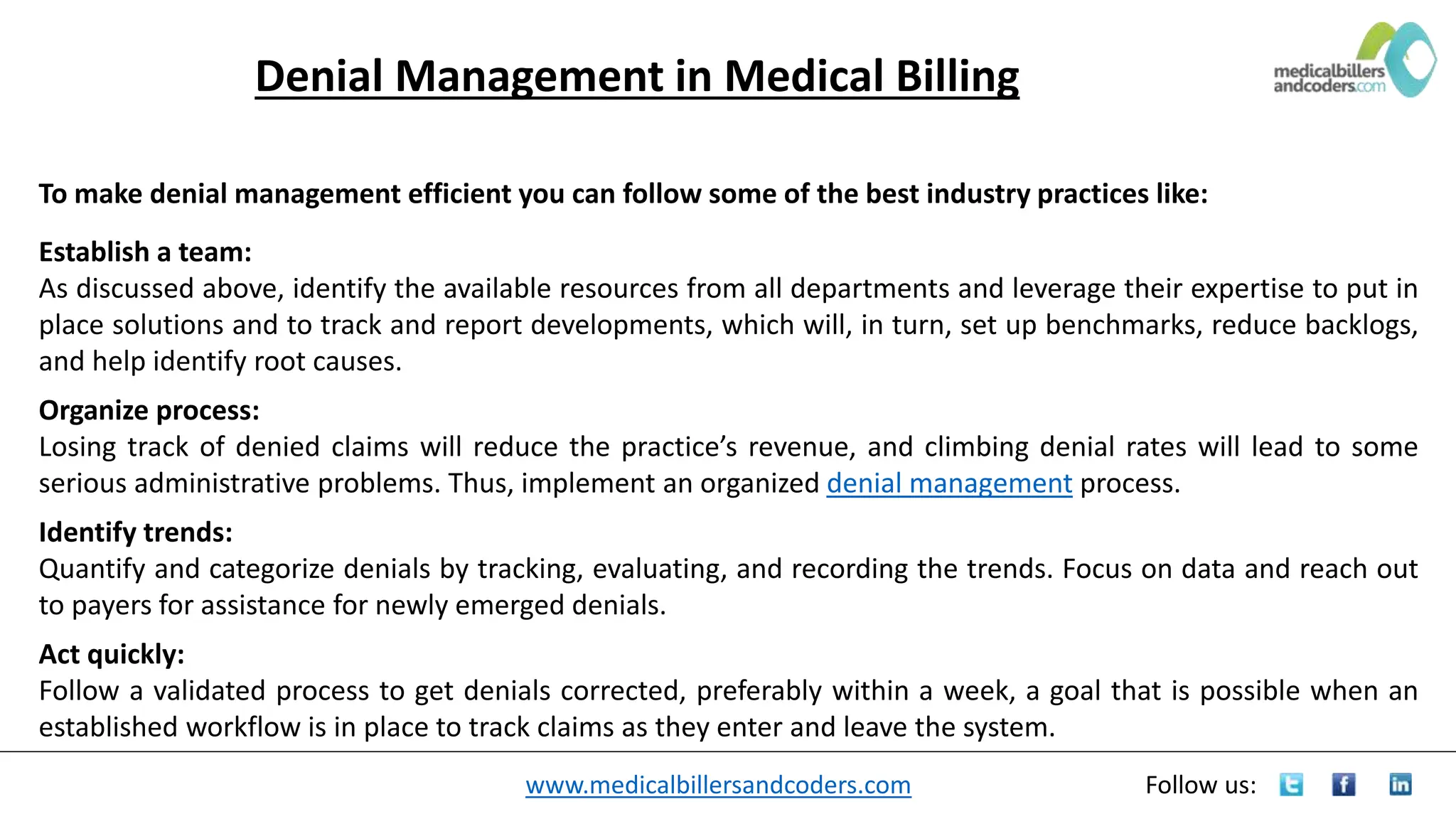
Several strategies can help healthcare providers minimize denials. These include: investing in robust billing software, providing comprehensive staff training, implementing rigorous claim scrubbing processes, and conducting regular audits of billing practices.
Proactive measures, such as verifying patient insurance eligibility before each visit and obtaining prior authorization when required, can also significantly reduce denials. Staying updated on coding changes and payer policies is crucial.
One rural clinic in Iowa, Dr. Emily Carter, implemented a new claim scrubbing system after experiencing a surge in denials related to coding errors. Within three months, the clinic saw a 20% reduction in claim denials, freeing up staff time and improving cash flow.
The Future of Medical Billing
The healthcare industry is increasingly embracing automation and artificial intelligence (AI) to improve billing accuracy and efficiency. AI-powered tools can help identify potential coding errors and compliance issues before claims are submitted.
Furthermore, initiatives like the Centers for Medicare & Medicaid Services' (CMS) efforts to promote interoperability are fostering greater transparency and data exchange between providers and payers. This ultimately aims to streamline the billing process and reduce denials.
While the medical billing landscape is constantly evolving, understanding the top causes of claim denials and implementing effective prevention strategies remains essential for healthcare providers' financial health and ability to provide quality patient care.