Which Of The Following Is A Gonadotropic Hormone

The intricate dance of hormones within the human body governs countless functions, from growth and development to reproduction. Among these vital chemical messengers, gonadotropic hormones play a critical role in regulating the reproductive systems of both males and females.
Understanding which hormones fall under this classification is crucial for comprehending the underlying mechanisms of fertility, puberty, and various reproductive disorders. This knowledge is essential not only for medical professionals but also for anyone seeking to gain a deeper understanding of their own physiology.
Gonadotropic Hormones: A Deep Dive
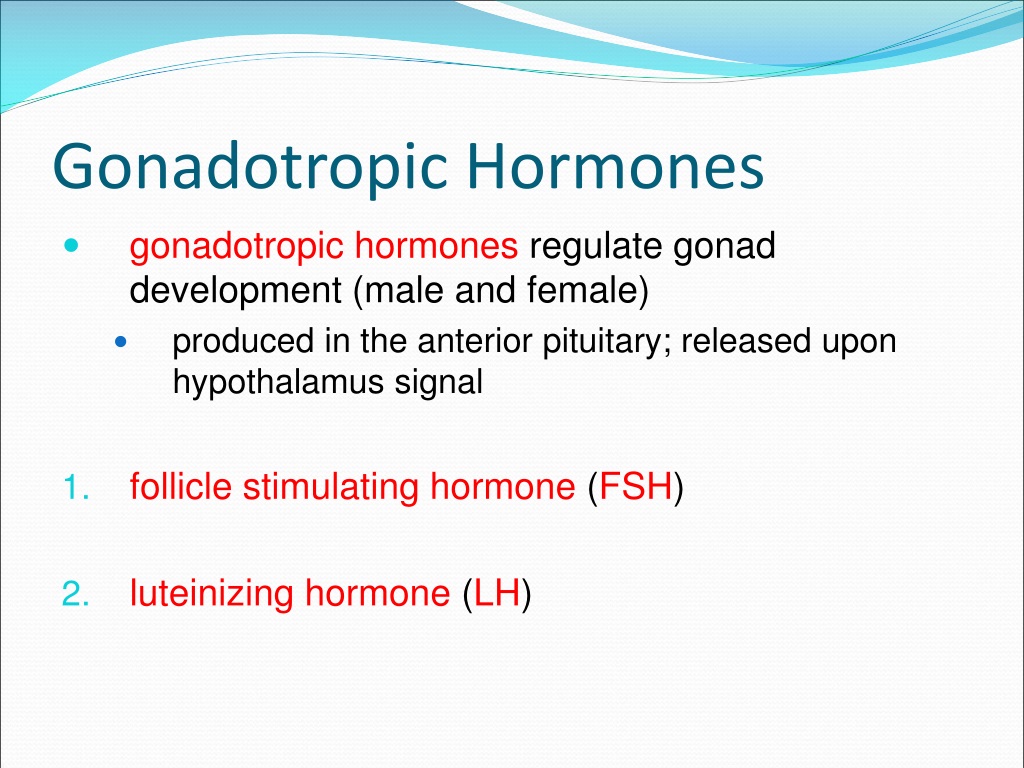
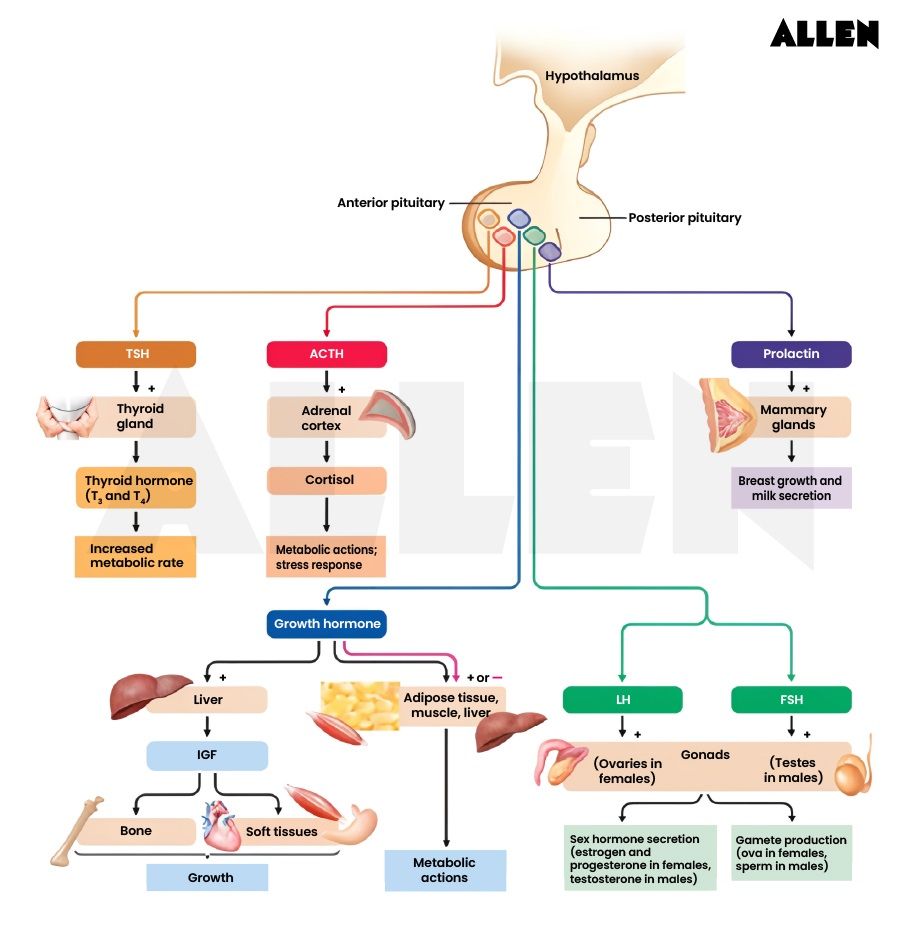
At its core, the question "Which of the following is a gonadotropic hormone?" requires a clear understanding of the term itself. Gonadotropic hormones are a group of hormones secreted by the anterior pituitary gland. These hormones act directly on the gonads (testes in males and ovaries in females) to regulate their function.
These vital hormones are fundamental for sexual development and reproductive capacity. Without them, key reproductive processes would be severely impaired or non-existent.
Follicle-Stimulating Hormone (FSH)
Follicle-stimulating hormone, or FSH, is undoubtedly a key gonadotropic hormone. In females, FSH stimulates the growth of ovarian follicles in the ovary before the release of an egg from one follicle at ovulation. It also promotes the production of estrogens, which are vital for the development of female secondary sexual characteristics and regulation of the menstrual cycle.
In males, FSH acts on Sertoli cells within the testes. These cells are crucial for supporting sperm maturation. FSH stimulates the production of androgen-binding protein, which helps concentrate testosterone in the testes, enabling proper spermatogenesis.
Luteinizing Hormone (LH)
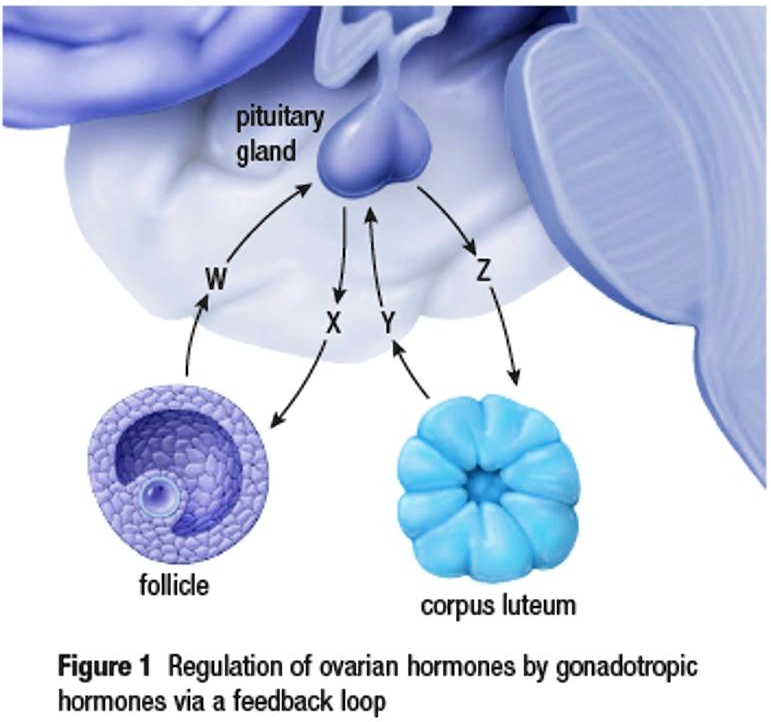
Another crucial gonadotropic hormone is luteinizing hormone, also known as LH. In females, LH triggers ovulation, the release of a mature egg from the ovarian follicle. Following ovulation, LH stimulates the ruptured follicle to develop into the corpus luteum, which produces progesterone, a hormone essential for maintaining pregnancy.
In males, LH stimulates the Leydig cells in the testes to produce testosterone. Testosterone, the primary male sex hormone, is essential for the development of male secondary sexual characteristics, such as deepening of the voice, growth of facial hair, and increased muscle mass. It also plays a vital role in spermatogenesis.
Human Chorionic Gonadotropin (hCG)
While FSH and LH are produced by the anterior pituitary gland, human chorionic gonadotropin, or hCG, deserves mention in the context of gonadotropic activity. hCG is a hormone produced by the placenta during pregnancy. Its primary function is to maintain the corpus luteum during early pregnancy, preventing it from degenerating.
By sustaining the corpus luteum, hCG ensures continued production of progesterone and estrogen. These hormones are essential for maintaining the uterine lining and supporting the developing embryo.
The Clinical Significance of Gonadotropic Hormones
Measuring gonadotropin levels is a common diagnostic tool in reproductive medicine. Abnormal levels of FSH and LH can indicate a range of underlying conditions.
For example, in women, elevated FSH levels can signal diminished ovarian reserve, a condition associated with decreased fertility and approaching menopause. In men, low LH and testosterone levels may indicate hypogonadism, a condition characterized by reduced testosterone production.
"Understanding the roles of gonadotropic hormones is paramount for diagnosing and treating infertility in both men and women," explains Dr. Emily Carter, a reproductive endocrinologist at the University of California, San Francisco.
Furthermore, synthetic versions of gonadotropic hormones are used in assisted reproductive technologies, such as in vitro fertilization (IVF). These hormones are administered to stimulate ovulation and increase the chances of successful conception.
Beyond Reproduction: Emerging Research
The influence of gonadotropic hormones extends beyond the reproductive system. Emerging research suggests potential links between these hormones and bone health, cognitive function, and even cardiovascular health.
For instance, studies have shown that decreased estrogen levels following menopause can contribute to bone loss and increased risk of osteoporosis. Similarly, testosterone deficiency in men has been linked to decreased bone density and muscle mass.
Future Directions
The ongoing exploration of gonadotropic hormones promises to reveal even more intricate connections between these hormones and overall health. Future research may focus on developing more targeted therapies for reproductive disorders, as well as exploring the potential of gonadotropic hormones for treating non-reproductive conditions.
A deeper understanding of these complex hormonal interactions could lead to innovative approaches for preventing and managing age-related diseases and improving the overall quality of life.