Can Edema Be Caused By Stress
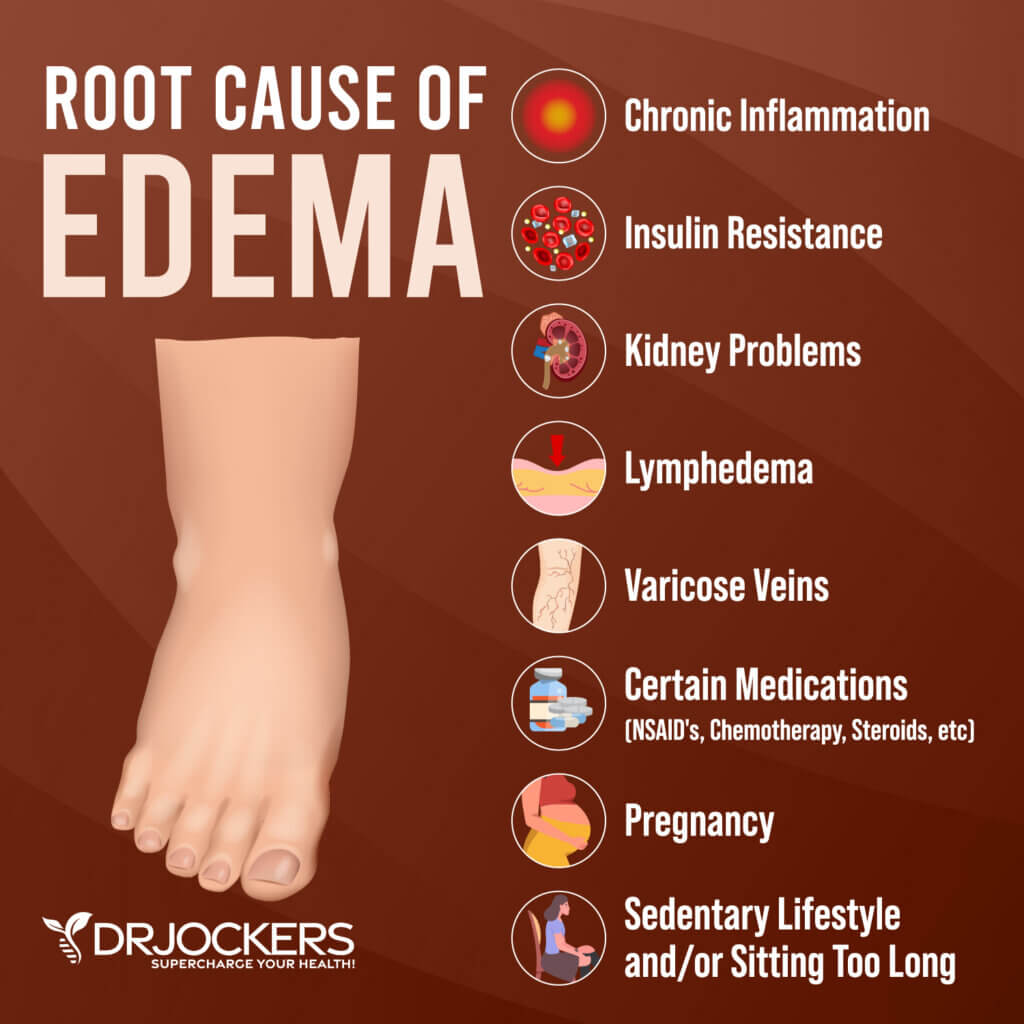
The sensation of puffiness, swelling, or tightness in the body, medically known as edema, is a common ailment that can stem from a variety of underlying causes. While conditions like heart failure, kidney disease, and pregnancy are well-established culprits, the potential role of stress in triggering or exacerbating edema is a subject of ongoing discussion and investigation.
This article delves into the complex relationship between stress and edema, exploring the physiological mechanisms through which psychological distress might contribute to fluid retention and swelling. It will examine the evidence, or lack thereof, supporting this connection, offering insights from medical experts and research findings.
Understanding Edema: A Brief Overview
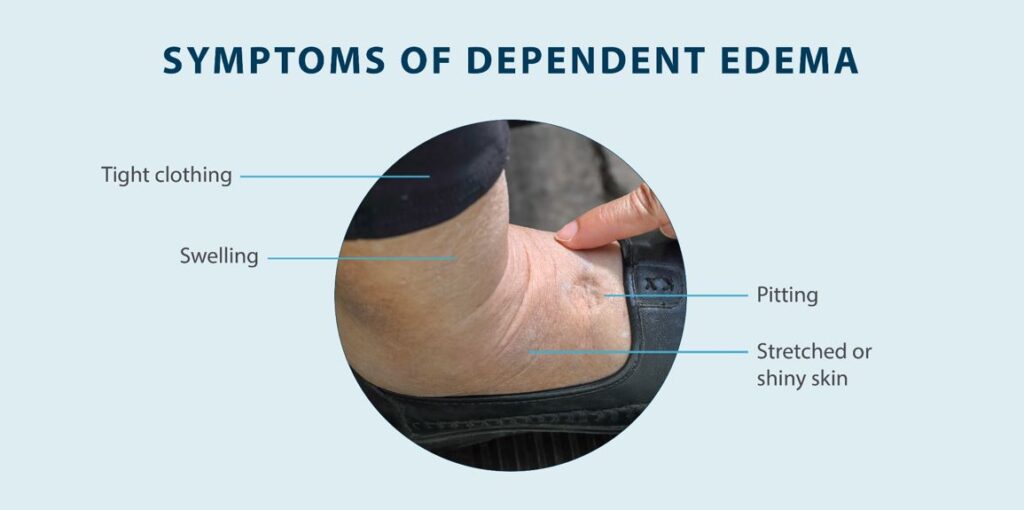
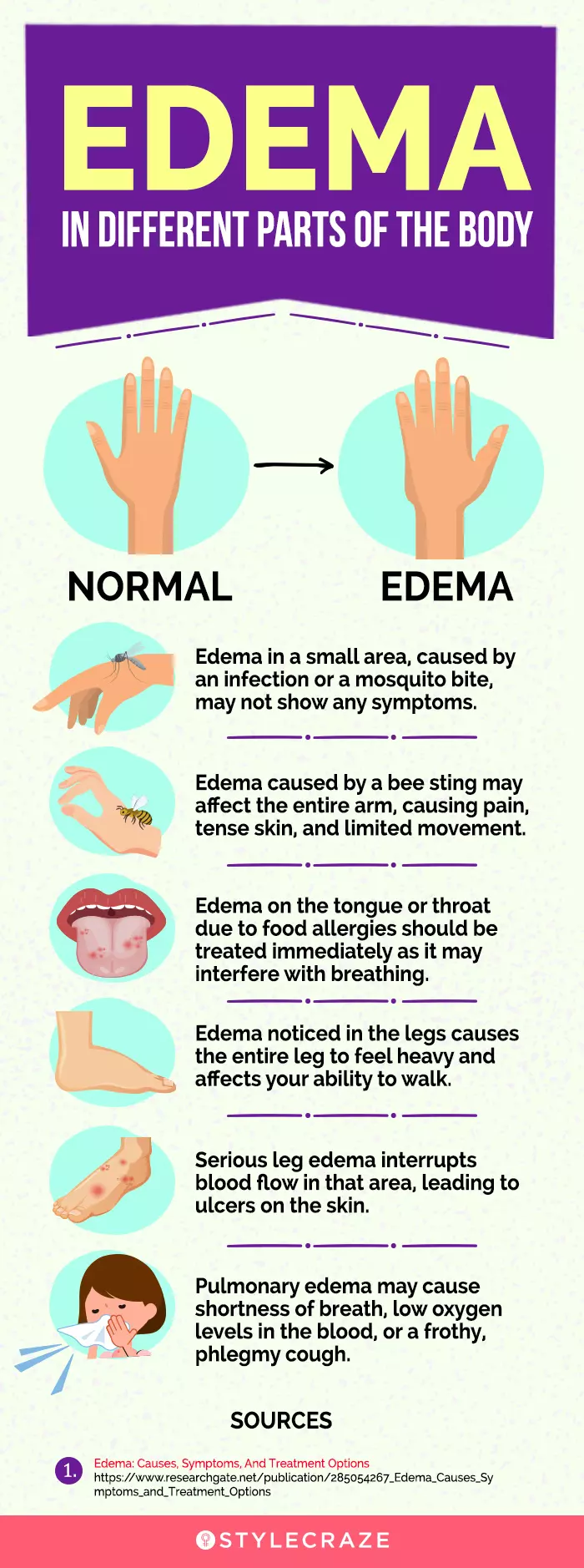
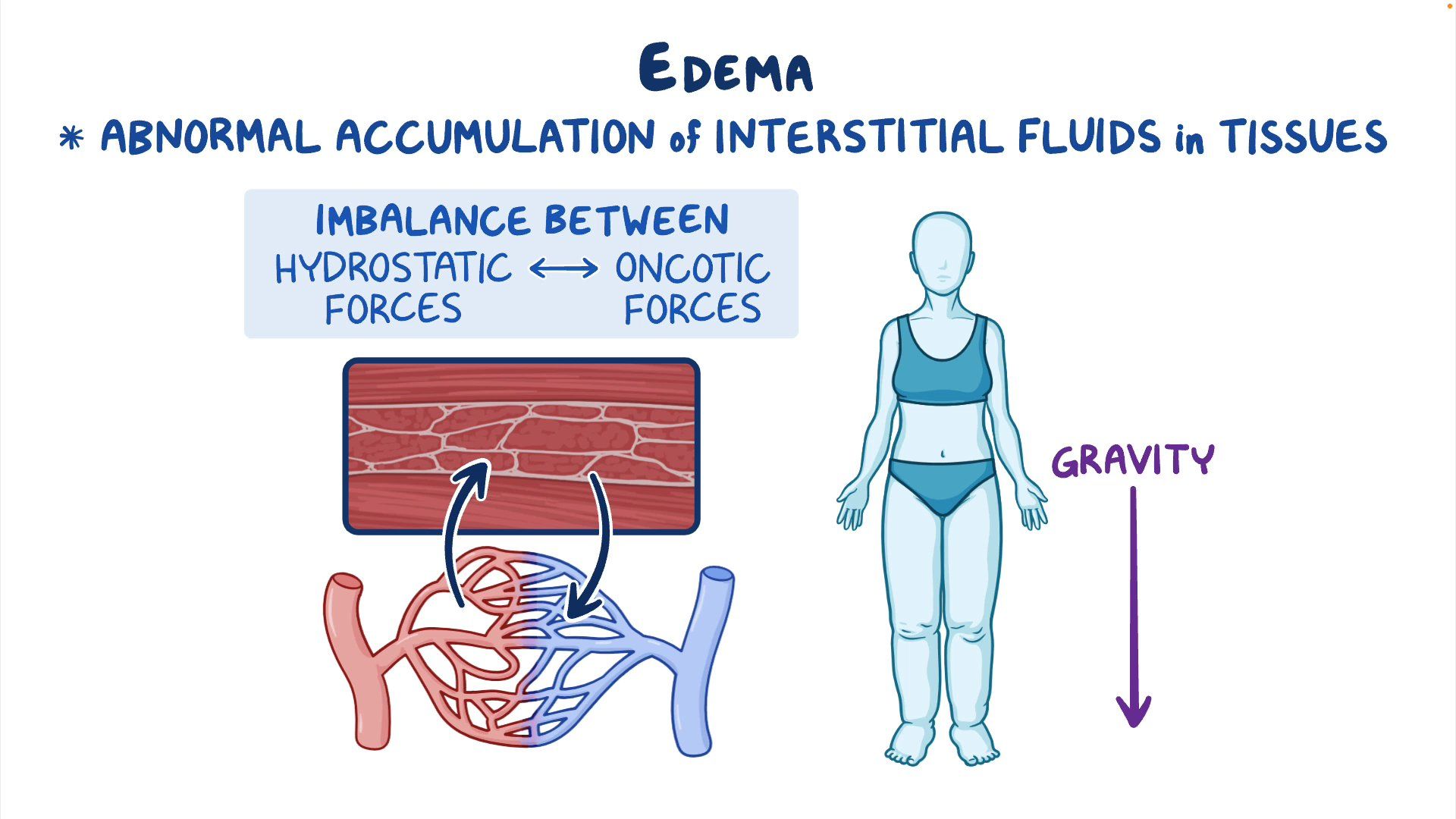
Edema occurs when excess fluid accumulates in the body's tissues. This fluid, primarily water, leaks from blood vessels into the surrounding spaces.
Symptoms can range from mild swelling in the ankles or feet to more widespread and severe fluid retention. While often harmless, edema can be a sign of a more serious medical condition.
The Stress Response and Its Physiological Effects
When faced with stress, the body activates the hypothalamic-pituitary-adrenal (HPA) axis, a complex neuroendocrine system. This activation triggers the release of stress hormones, most notably cortisol.
Cortisol, while essential for managing stress, can have a cascade of effects on the body. These effects include alterations in blood pressure, blood sugar levels, and immune function.
The Potential Link Between Stress and Edema
While direct causation is difficult to prove, several pathways suggest a potential link between stress and edema. Changes in hormone levels may contribute to fluid retention.
Chronic stress can lead to increased levels of Antidiuretic Hormone (ADH), also known as vasopressin. ADH prompts the kidneys to retain more water, potentially contributing to edema.
Stress can also influence the vascular system. Prolonged stress may contribute to inflammation, which can compromise the integrity of blood vessels, making them more prone to leakage.
Furthermore, stress can exacerbate existing conditions that cause edema. For example, individuals with heart or kidney problems may experience worsened symptoms during periods of heightened stress.
What the Experts Say
Dr. Anya Sharma, a nephrologist at the Mayo Clinic, stated, "While stress itself is unlikely to be the sole cause of significant edema, it can certainly exacerbate underlying conditions that contribute to fluid retention. We often see patients with existing heart or kidney issues experiencing a worsening of their edema symptoms during periods of high stress."
Dr. David Lee, an endocrinologist at Massachusetts General Hospital, adds, "The interplay between stress hormones, particularly cortisol and ADH, and their impact on fluid balance is complex. More research is needed to fully understand the extent to which chronic stress can directly contribute to edema in otherwise healthy individuals."
According to the American Heart Association, managing stress is crucial for overall cardiovascular health. Uncontrolled stress can negatively impact blood pressure and contribute to other risk factors for heart disease, a leading cause of edema.
Lifestyle Factors and Stress Management
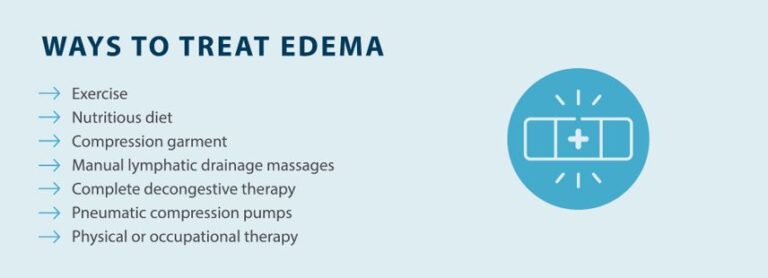
Addressing lifestyle factors plays a crucial role in managing both stress and potentially mitigating any associated edema. A balanced diet with reduced sodium intake can help regulate fluid balance.
Regular physical activity can reduce stress and improve circulation. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Stress management techniques such as meditation, yoga, and deep breathing exercises can help regulate the HPA axis and reduce cortisol levels. Prioritizing sleep and ensuring adequate rest is also essential for managing stress.
When to Seek Medical Attention
While stress-related edema is generally mild and temporary, it's important to consult a healthcare professional if you experience sudden or severe swelling. Seek immediate medical attention if edema is accompanied by shortness of breath, chest pain, or difficulty breathing.
These symptoms could indicate a serious underlying medical condition. It is better to err on the side of caution.
It is also crucial to consult with a physician or other healthcare provider to review your medications. Certain medications can cause edema or exacerbate existing conditions.
Conclusion
While direct evidence definitively linking stress as a sole cause of edema remains limited, the physiological mechanisms through which stress can influence fluid balance suggest a potential connection. Managing stress through lifestyle modifications and relaxation techniques is a worthwhile endeavor for overall health and may help mitigate mild edema symptoms.
However, persistent or severe edema warrants medical evaluation to rule out underlying medical conditions. It is important to approach the topic with a balanced perspective.
Further research is needed to fully elucidate the complex relationship between stress and edema, ultimately providing more targeted and effective interventions for individuals experiencing fluid retention.





:max_bytes(150000):strip_icc()/common-causes-of-foot-and-ankle-swelling-1337777-5c04ad02c9e77c0001b0f9e0.png)