Causes Of Death After Stem Cell Transplant

Stem cell transplants, a potentially life-saving procedure for individuals battling blood cancers and other severe diseases, come with inherent risks. While the procedure aims to replace damaged or diseased cells with healthy ones, understanding the common causes of mortality post-transplant is crucial for improving patient outcomes and informing clinical practice.
This article examines the primary causes of death following stem cell transplantation, based on recent research and data from reputable medical organizations. It will explore the complexities of this treatment and the factors that contribute to patient mortality.
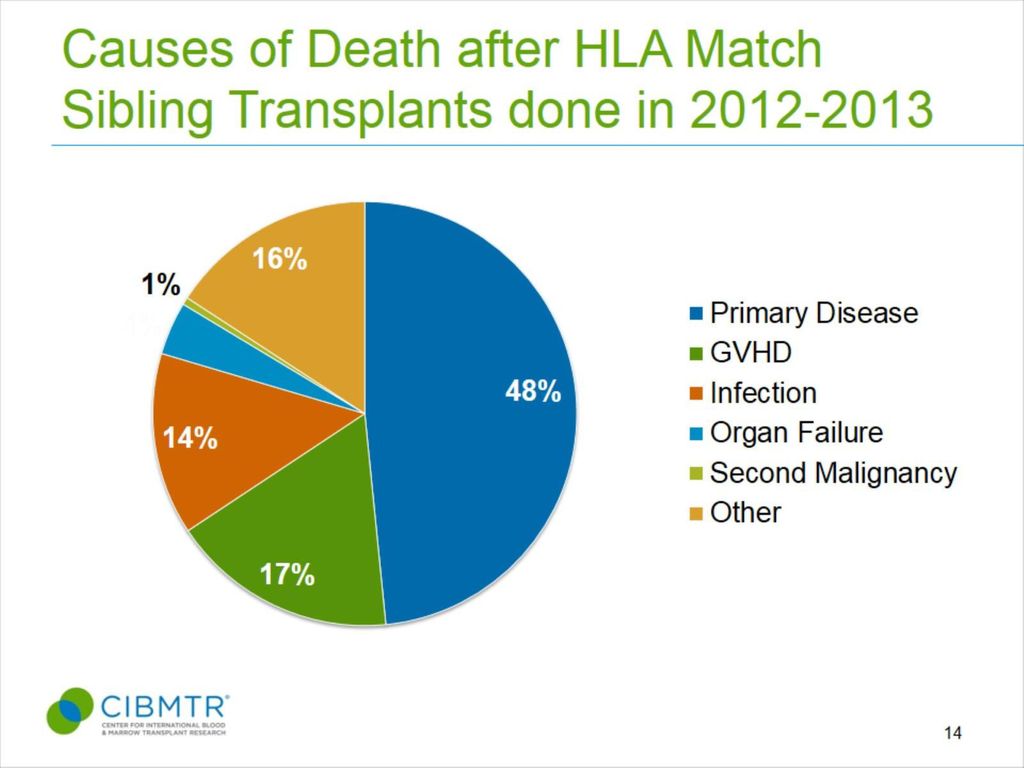
Leading Causes of Mortality
According to various studies and reports from organizations like the National Institutes of Health (NIH) and the American Society for Transplantation and Cellular Therapy (ASTCT), several factors contribute significantly to mortality after stem cell transplants. These factors include graft-versus-host disease (GVHD), infections, relapse of the underlying disease, and organ failure.
Graft-versus-Host Disease (GVHD)
GVHD is a major complication where the transplanted donor cells (the graft) attack the recipient's tissues (the host). This immune response can manifest in various organs, including the skin, liver, and gastrointestinal tract.
Acute GVHD typically occurs within the first 100 days post-transplant, while chronic GVHD can develop later. The severity of GVHD ranges from mild to life-threatening, and its management often involves immunosuppressive medications.
Despite advancements in GVHD prevention and treatment, it remains a leading cause of morbidity and mortality. Effective strategies to prevent and manage GVHD are critical to improving post-transplant survival.
Infections
Patients undergoing stem cell transplants are highly susceptible to infections due to the immunosuppressive regimens used to prevent GVHD and the period of neutropenia (low white blood cell count) that follows transplantation. Infections can be bacterial, viral, or fungal.
Common bacterial infections include pneumonia and bloodstream infections, while viral infections such as cytomegalovirus (CMV) and adenovirus can also pose significant risks. Invasive fungal infections, such as aspergillosis, are another serious concern.
Prophylactic measures, such as antiviral and antifungal medications, are often used to prevent infections. However, prompt diagnosis and aggressive treatment are essential when infections occur, as they can rapidly become life-threatening.
Relapse of the Underlying Disease
Despite successful engraftment, the underlying disease for which the transplant was performed can relapse. This is a significant cause of mortality, particularly in patients with advanced or aggressive cancers.
The risk of relapse varies depending on the type of disease, the stage at the time of transplant, and the conditioning regimen used. Minimal residual disease (MRD) monitoring can help detect early signs of relapse.
Strategies to prevent relapse include post-transplant maintenance therapy and donor lymphocyte infusions (DLI), which can boost the graft's anti-tumor effect. However, these approaches also carry the risk of GVHD.
Organ Failure
Organ failure, including liver, kidney, and heart failure, can occur as a consequence of the transplant process or related complications. The intensive conditioning regimens used prior to transplant can damage organs.
GVHD can also contribute to organ dysfunction, particularly liver GVHD. Veno-occlusive disease (VOD), a condition affecting the liver's small blood vessels, is another potential cause of liver failure after transplant.
Careful monitoring of organ function and prompt intervention are crucial for managing organ failure. In some cases, organ transplantation may be necessary.
Other Contributing Factors
Besides the primary causes mentioned above, other factors can contribute to post-transplant mortality. These include pulmonary complications such as idiopathic pneumonia syndrome (IPS) and diffuse alveolar hemorrhage (DAH).
Delayed engraftment, where the transplanted cells fail to properly establish themselves in the bone marrow, can also increase the risk of infections and other complications. Older age and comorbidities (other health conditions) can also increase mortality risk.
Advances in supportive care, such as improved antimicrobial agents and better GVHD prophylaxis, have helped to reduce mortality rates. However, ongoing research is needed to further improve outcomes.
The Importance of Continued Research
Understanding the causes of death after stem cell transplantation is vital for improving patient outcomes. Research efforts are focused on developing more effective strategies to prevent and manage GVHD, infections, and relapse.
Personalized approaches to transplant, tailored to the individual patient's disease and risk factors, are also being explored. This includes optimizing conditioning regimens, selecting the most appropriate donor, and using targeted therapies to prevent relapse.
Collaboration among researchers, clinicians, and patients is essential for advancing the field of stem cell transplantation and improving the lives of those who undergo this potentially life-saving procedure.
The information presented here is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with qualified healthcare professionals for any health concerns or before making any decisions related to your health or treatment. The data and statistics mentioned may vary based on specific studies and patient populations.













30404-X/asset/20f12640-959c-43ba-8f80-442cfe26f129/main.assets/gr1_lrg.jpg)


