Good Health Distribution Partners First Health Network

The complex landscape of healthcare access in America is undergoing a significant shift, with ripples felt across the nation's insurance providers and the millions they serve. At the heart of this transformation lies the evolving relationship between Good Health Distribution Partners (GHDP), a major player in pharmaceutical distribution, and First Health Network, a broad-reaching provider network owned by CVS Health.
The core issue centers on recent contract negotiations and subsequent network participation changes affecting First Health Network's accessibility for individuals covered by health plans utilizing GHDP's pharmaceutical offerings. This situation has raised concerns among patients, healthcare professionals, and industry analysts regarding potential disruptions in care, particularly for those relying on specialized medications or treatments.
Understanding Good Health Distribution Partners
GHDP is a leading distributor of pharmaceuticals and healthcare products, connecting manufacturers with pharmacies, hospitals, and other healthcare providers. Their expansive reach makes them a crucial link in the supply chain, ensuring medications are available to patients nationwide.
The company's operations are vital for ensuring the timely and efficient delivery of prescription drugs, including specialty medications often used to treat complex conditions.
First Health Network: A Wide-Reaching Provider Network
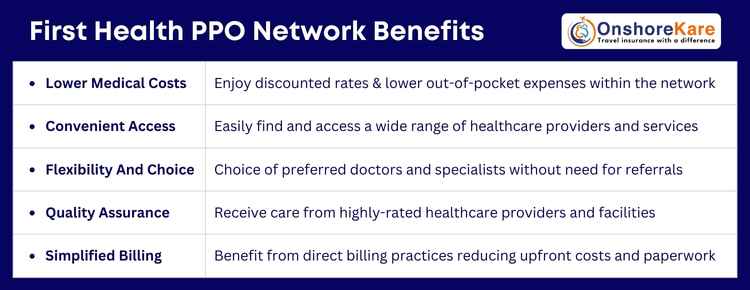
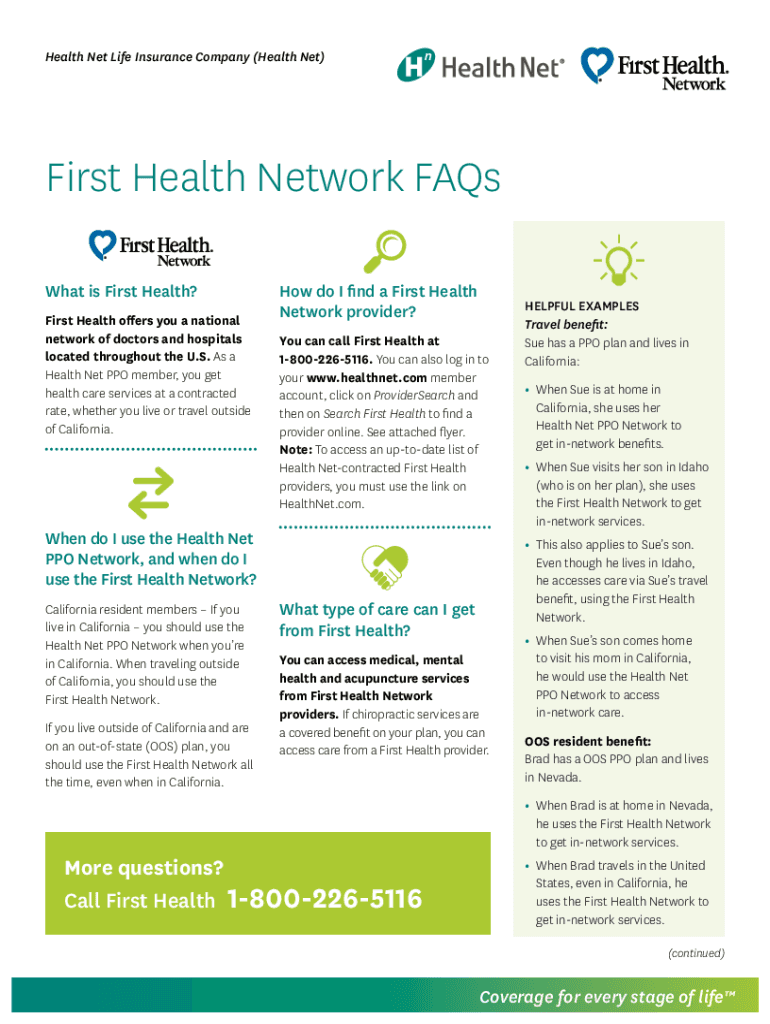
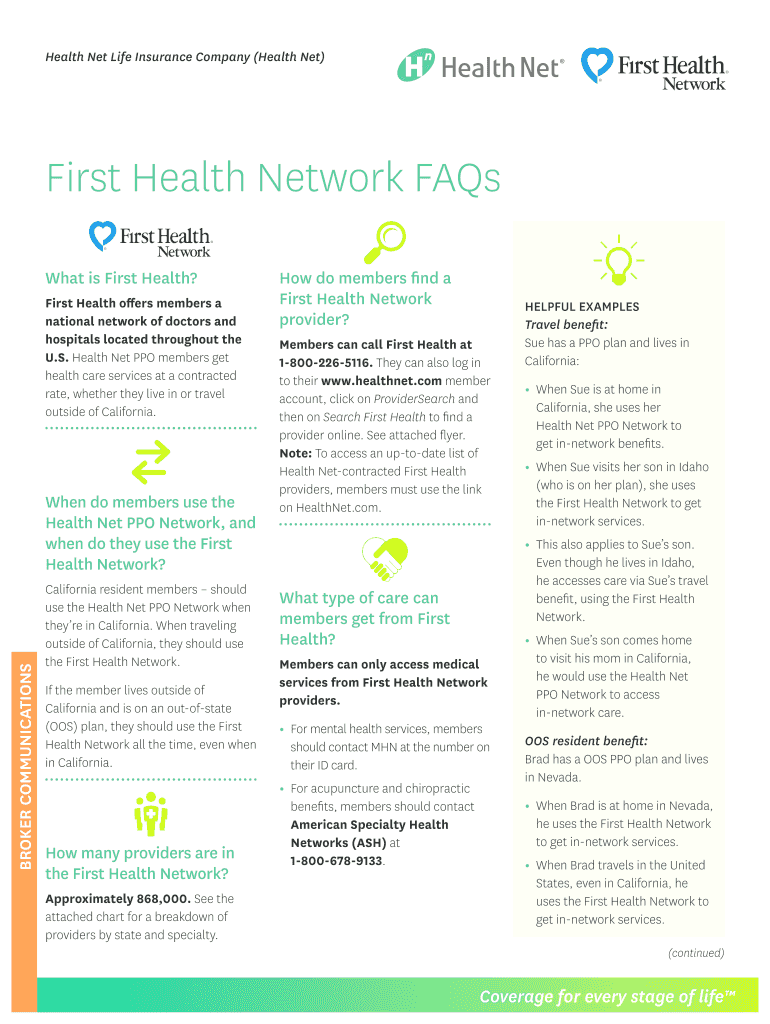
First Health Network, owned by CVS Health, is a significant provider network offering access to a broad range of physicians, hospitals, and other healthcare facilities. Their network spans across the United States, providing coverage for millions of individuals through various health plans.
This extensive network is particularly important for individuals living in rural or underserved areas, where access to specialized care might be limited.
The Contract Negotiation Impasse
Recent contract negotiations between GHDP and First Health Network have reportedly reached an impasse, leading to changes in network participation for certain health plans utilizing GHDP's services. The specific details of the negotiations remain confidential, but sources indicate disagreements over reimbursement rates and contract terms.
This disagreement has resulted in some patients finding that their preferred providers are no longer considered "in-network" under their current health plans.
Potential Impact on Patients
The primary concern stemming from this situation is the potential disruption of care for patients who rely on First Health Network providers. Patients may be forced to switch doctors, travel longer distances for treatment, or face higher out-of-pocket costs if they choose to remain with their current providers as "out-of-network" options.
This is especially concerning for individuals with chronic conditions or those requiring specialized medical care, as continuity of care is crucial for managing their health effectively.
"Any disruption in access to care is a serious concern," says Dr. Emily Carter, a healthcare policy analyst. "Patients need stability and predictability in their healthcare coverage, and these types of contract disputes can undermine that."
The Role of CVS Health
As the owner of First Health Network, CVS Health plays a crucial role in resolving the current situation. CVS Health has publicly stated its commitment to ensuring access to affordable healthcare and is actively working to find a resolution with GHDP.
The company is also providing resources to help patients navigate the changes and find alternative in-network providers.
Industry Perspectives
Healthcare industry experts suggest that the dispute between GHDP and First Health Network reflects a broader trend of increasing tension between pharmaceutical distributors and provider networks. Negotiations over drug pricing and reimbursement rates are becoming more complex as healthcare costs continue to rise.
These experts suggest that finding a sustainable solution requires a collaborative approach that addresses the financial pressures faced by both parties while prioritizing patient access to care.
Alternative Perspectives
Some industry observers argue that the shift in network participation could also drive greater efficiency and cost-effectiveness within the healthcare system. By negotiating more favorable terms with providers, health plans may be able to lower premiums and improve the overall affordability of healthcare.
However, this perspective emphasizes the importance of ensuring that cost-saving measures do not come at the expense of patient access or quality of care.
Moving Forward: Potential Solutions
Several potential solutions have been proposed to address the current situation. These include continued negotiations between GHDP and First Health Network, mediation by a third party, or regulatory intervention to ensure patient access to care.
Ultimately, a resolution that balances the financial interests of both parties with the needs of patients is essential for maintaining a stable and accessible healthcare system.
The Future of Healthcare Access
The ongoing situation between GHDP and First Health Network highlights the complexities and challenges facing the healthcare industry in the United States. As healthcare costs continue to rise and the demand for quality care increases, finding innovative solutions to ensure affordable and accessible healthcare for all remains a top priority.
The outcome of these negotiations will likely set a precedent for future relationships between pharmaceutical distributors and provider networks, shaping the landscape of healthcare access for years to come.
The coming weeks and months will be critical in determining the long-term impact of these events on patients and the healthcare system as a whole. Monitoring the situation closely and advocating for patient-centered solutions is paramount.