Which Of The Following Is Not True About Doctor Screenings
The routine doctor visit, a cornerstone of preventative medicine, is often accompanied by a battery of screenings. These tests, designed to detect diseases early, play a crucial role in maintaining public health. However, misinformation and misunderstandings surrounding the efficacy and appropriateness of certain screenings can lead to anxiety, unnecessary procedures, and misallocation of healthcare resources.
This article delves into the complexities of doctor screenings, examining common misconceptions and highlighting evidence-based recommendations. Our aim is to clarify which statements about doctor screenings are untrue, providing readers with the information they need to make informed decisions about their healthcare.
The Screening Landscape: What's Generally Accepted
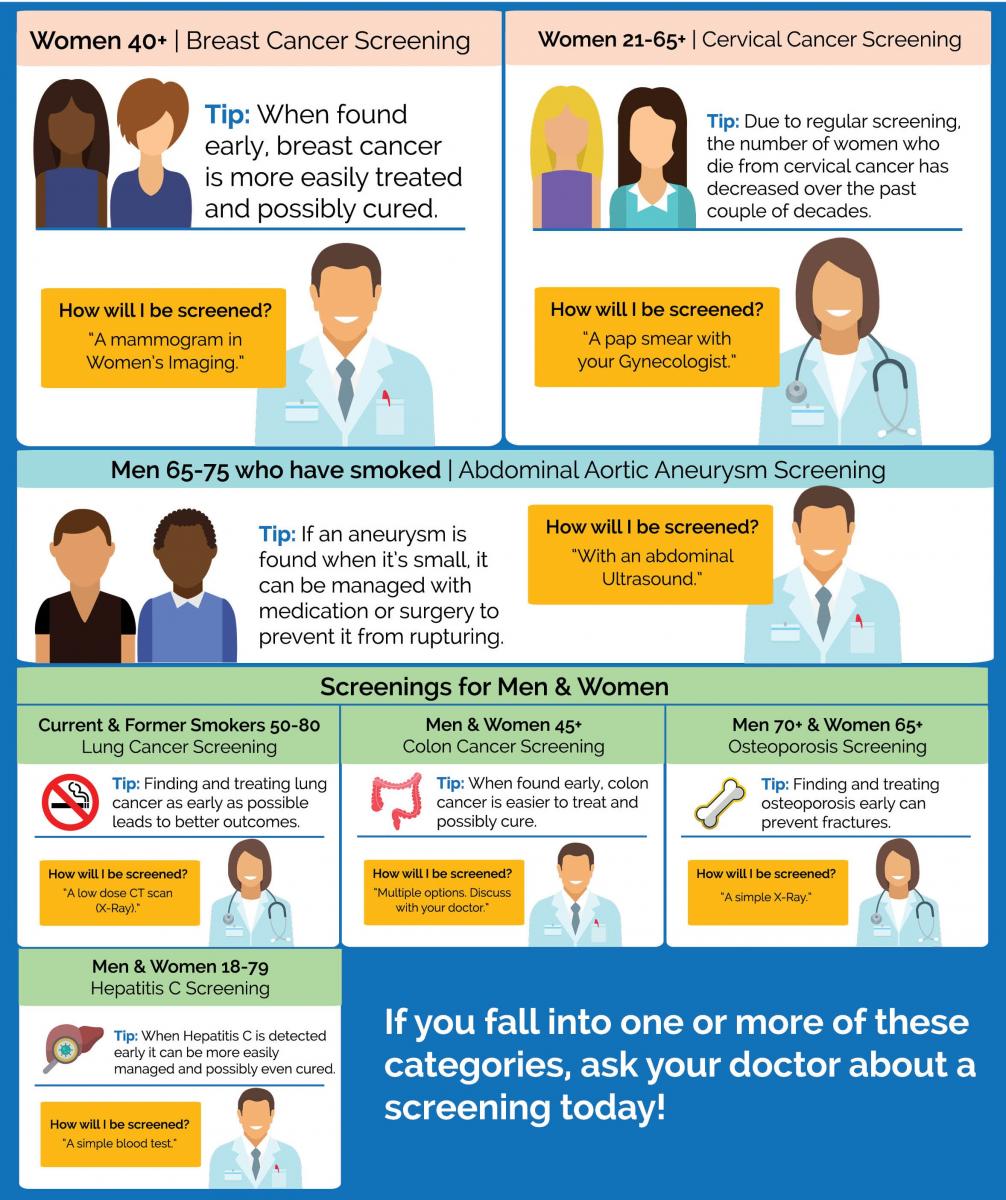
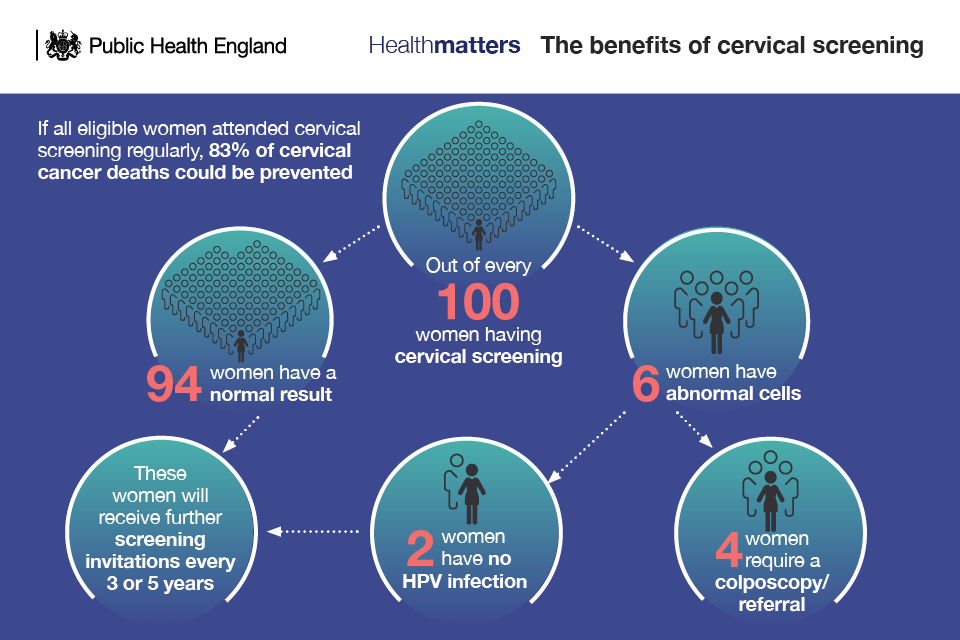
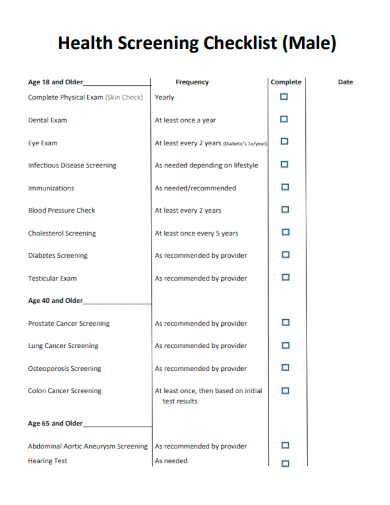
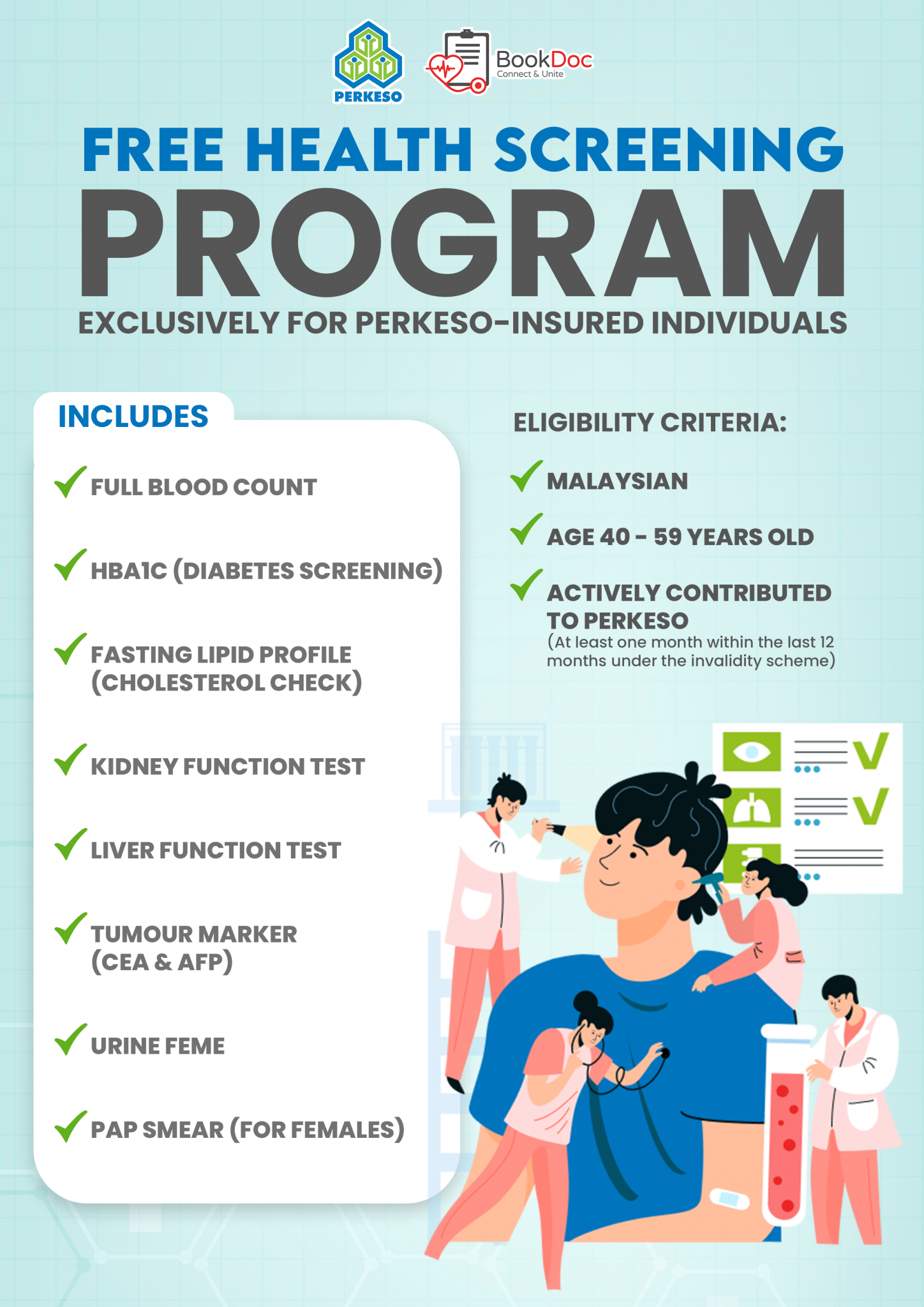
Before dissecting the myths, it's essential to understand what doctor screenings typically entail. Common screenings include those for blood pressure, cholesterol, certain cancers (like breast, cervical, and colon cancer), and diabetes. The goal is to identify potential health issues before symptoms appear, allowing for earlier intervention and potentially better outcomes.
The U.S. Preventive Services Task Force (USPSTF), an independent panel of experts, provides evidence-based recommendations on preventative services, including screenings. These recommendations are widely respected and often guide clinical practice.
Mythbusting: Separating Fact from Fiction
False Claim #1: More Screenings Are Always Better
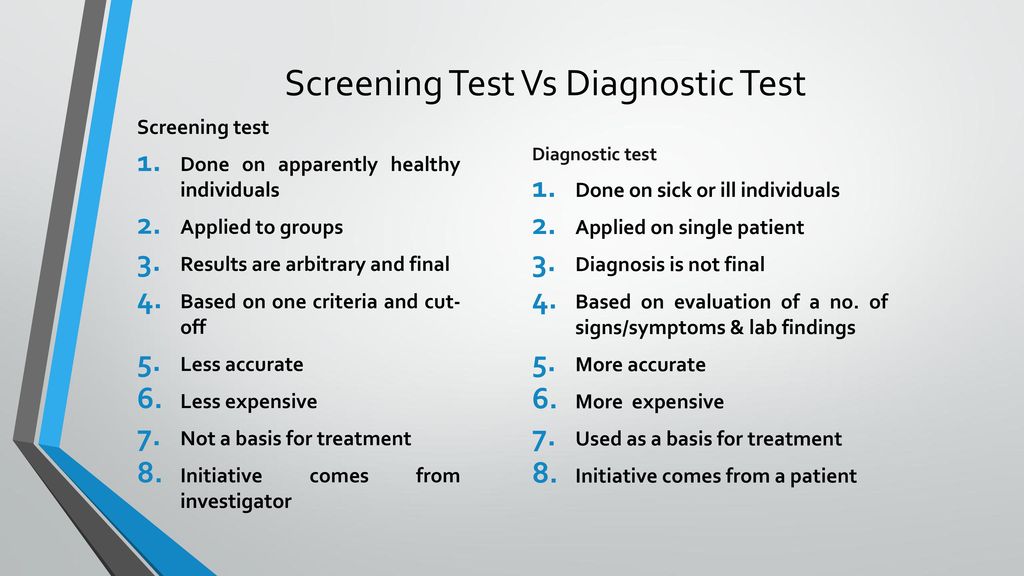
One prevailing misconception is that undergoing every available screening guarantees better health. This is demonstrably false. Over-screening can lead to false positives, resulting in unnecessary anxiety, further testing, and potentially invasive procedures like biopsies.
The harm of over-diagnosis, where a condition is identified that would never have caused problems during a person's lifetime, is a serious concern. For example, some prostate cancers detected through screening are slow-growing and may not require treatment, but the diagnosis can still cause significant stress and lead to potentially harmful interventions.
False Claim #2: Screening Guarantees You Won't Get a Disease
Screenings are not foolproof. They are designed to detect potential problems, but they are not 100% accurate. A negative screening result does not guarantee that a person is disease-free.
False negatives can occur, where a screening misses an existing condition. This can delay diagnosis and treatment, potentially leading to poorer outcomes. It's crucial to understand the limitations of each screening and to continue to monitor your health and report any new symptoms to your doctor.
False Claim #3: All Screenings Are Appropriate for Everyone at the Same Age
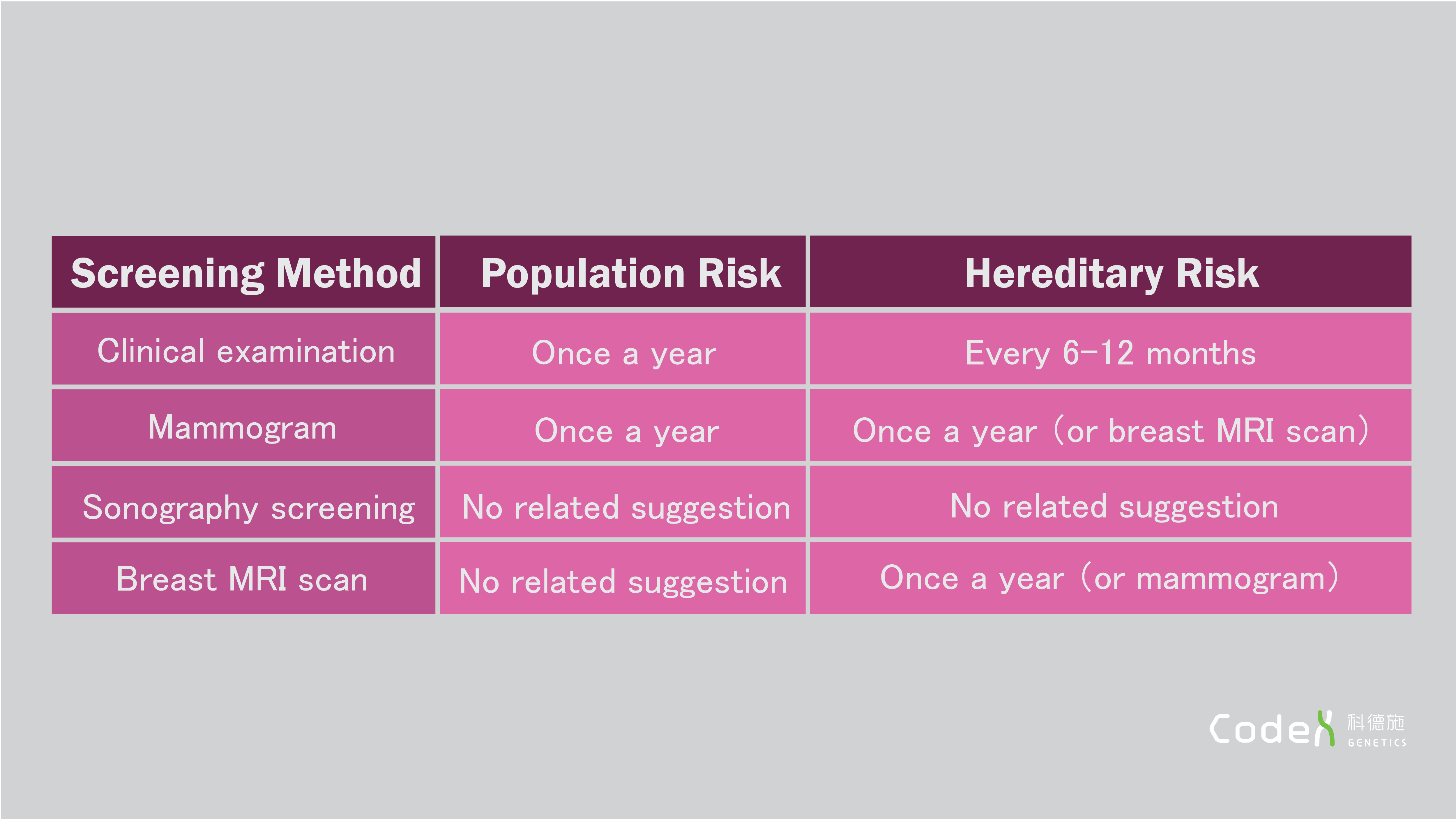
Age is a factor in screening recommendations, but it's not the only one. Individual risk factors, such as family history, lifestyle choices, and pre-existing conditions, play a significant role in determining which screenings are appropriate and when they should begin. The USPSTF provides age-specific recommendations, but these are meant to be guidelines, not rigid rules.
For instance, someone with a strong family history of colon cancer might need to start screening earlier than the recommended age of 45. Similarly, individuals with certain genetic predispositions may require more frequent or specialized screenings.
False Claim #4: If a Screening is Available, It Must Be Beneficial
The availability of a screening test doesn't automatically equate to its benefit. Some screenings lack sufficient evidence to demonstrate a clear improvement in health outcomes or may carry risks that outweigh the potential benefits. Furthermore, the cost-effectiveness of certain screenings needs to be carefully considered.
New screening technologies emerge constantly, but they should be thoroughly evaluated before being widely adopted. It's important to discuss the evidence supporting any new screening with your doctor and understand its potential benefits and risks.
The Importance of Personalized Screening Strategies
The key takeaway is that doctor screenings should be tailored to each individual's specific needs and risk factors. A "one-size-fits-all" approach is not only ineffective but can also be harmful. Open communication with your doctor is essential to developing a personalized screening plan.
Your doctor can assess your individual risk factors, discuss the potential benefits and risks of different screenings, and help you make informed decisions about your healthcare. Shared decision-making, where both the doctor and patient actively participate in the decision-making process, is crucial.
According to the National Institutes of Health (NIH), shared decision making improves patient satisfaction and adherence to treatment plans.
Moving Forward: Towards Informed Healthcare Choices
In conclusion, while doctor screenings play a vital role in preventative medicine, it's crucial to approach them with a discerning eye. Misconceptions about screenings can lead to unnecessary anxiety and potentially harmful interventions. Remember that more screenings are not always better, screenings aren't guarantees, and individual risk factors should guide screening decisions.
By engaging in open communication with your doctor and understanding the evidence-based recommendations for preventative care, you can make informed choices that promote your long-term health and well-being. Staying informed about the latest guidelines from organizations like the USPSTF and the NIH is a crucial step towards proactive healthcare.